Overview of Monoclonal B-cell Lymphocytosis
Monoclonal B-cell Lymphocytosis (MBL) is not cancer, but is considered a risk factor for developing Chronic Lymphocytic Leukaemia. (CLL). However, most people with MBL will never progress to CLL.
MBL develops when your body makes too many blood cells called B-cell lymphocytes. This happens when one abnormal B-cell clones itself many times, so all the extra B-cells made from that one abnormal cell are also abnormal, and create more clones.
Lymphocytes are part of our immune system and fight infection and disease. They also identify when cells are not developing right, and help them to either repair themselves or destroy the abnormal cells.
While you may have extra B-cells, it does not help your immune system because they are too abnormal to work properly. However, because these cells are cloned from a single abnormal B-cell, you still have healthy B-cells too.
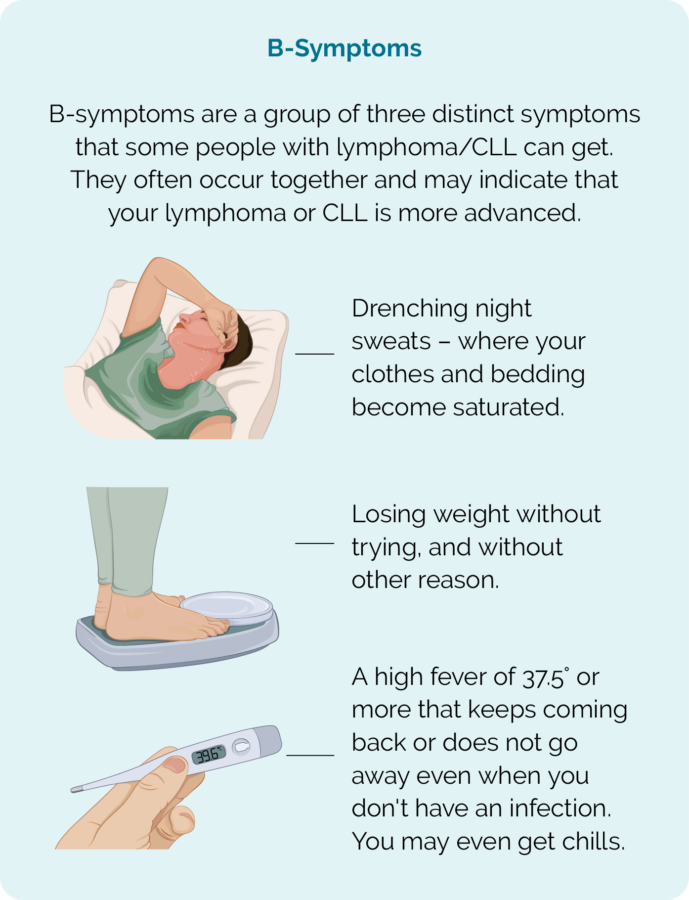
You will not have any symptoms with MBL, however if your MBL progresses into CLL you may get B-symptoms. Click here to learn about B-symptoms.
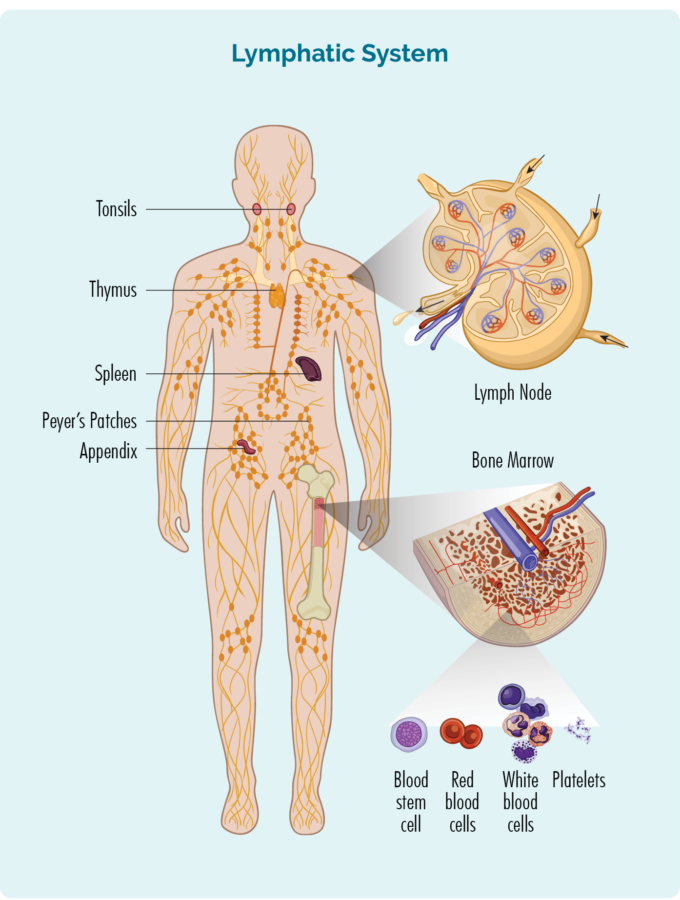
Unlike other blood cells, lymphocytes live mostly in our lymphatic system, with only a small number in our blood. The lymphocytes affected by MBL and CLL are in your blood and bone marrow.
Types of Monoclonal B-cell Lymphocytosis (MBL)
There are two subtypes of Monoclonal B-cell Lymphocytosis (MBL). These include low count and high count MBL.
- Low count MBL is when the number of abnormal lymphocytes in your bloodstream are less than 5000 (<0.5 x 10⁹/L). Low count MBL does not progress to CLL.
- High count MBL is when the number of abnormal lymphocytes detected in your bloodstream are more than 5000 (>0.5 x 10⁹/L). High count MBL has a rare chance (around 1-2%) each year of progressing to CLL.
MBL is said to have transformed to CLL if the abnormal lymphocyte count in the blood (lymphocytosis) reaches levels of more than 5 x 10⁹/L.
How is MBL similar to CLL?
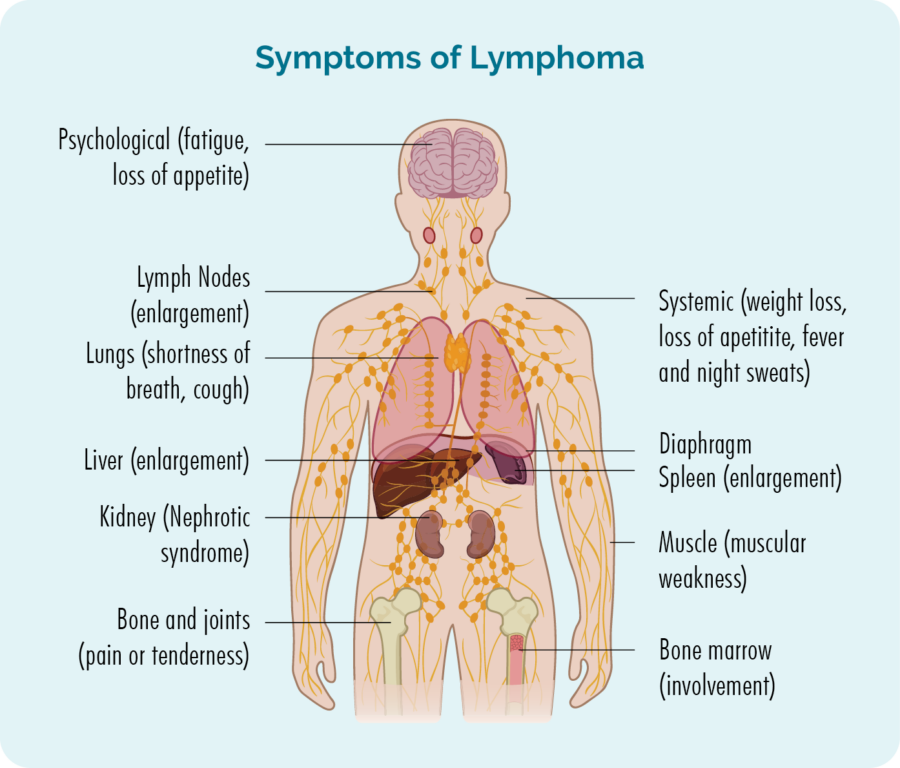
The monoclonal B-cell lymphocytes in high count MBL have the same proteins on them that are found on the cells of people with CLL. This is why MBL is thought to increase your risk of developing CLL. However, with MBL, you will have less monoclonal B-cells and not have any symptoms. If it progresses to CLL, you will have a lot more abnormal monoclonal B-cells, and may start to develop symptoms of lymphoma.
Who develops MBL?
You are more likely to develop MBL as you get older. It is very rare in people less than 40 years of age, but about 1 in 10 people over 40 years will have MBL. This increases even more in people over 90 years of age, with about 7-8 out of every 10 people over 90 years having MBL.
Other risk factors for developing MBL include:
- At least two people in your family have had Chronic Lymphocytic Leukaemia (CLL)
- If you’ve ever had certain infections such as hepatitis C, pneumonia, influenza, cellulitis, upper respiratory tract infections and herpes zoster.
- MBL is more common in men than in women, though women can still get it.
If you have a high count MBL and it progresses on to become CLL, you still may not need treatment. About one in five people with CLL will never need any treatment. Most people who progress to CLL will still live a normal life and have a normal life span.
How is MBL diagnosed?
MBL does not cause symptoms, so you may only find out their is an issue when you have a blood test for some other reason, that shows you have a high level of B-cell lymphocytes in your blood. However, there are several other reasons your lymphocyte count can be raised. These can include infection, inflammation and auto immune disorders.
Your doctor will likely recheck your blood tests over the next three months to see if the lymphocyte count returns to normal. If the level remains high or gets higher, you may need more tests to find out why.
Flow cytometry
Flow cytometry is a special test done in pathology on your blood tests, and can be used to diagnose MBL. It looks more closely at the cells to see all the different characteristics of the cells, including the types of proteins they have on them. It will show if the extra B-cells have all been cloned from the same original cell (monoclonal), and if the proteins are the same ones found on CLL cells.
The pathologist will also be able to identify how many of your B-cells are abnormal monoclonal cells and how many are normal, which will help them work out if you have MBL or CLL.
Other tests
You may need more tests to make sure the abnormal cells are only in you blood and are not in you lymph nodes or other parts of your body. This is to rule out CLL or other types of lymphoma as a cause for the high monoclonal B-cell count.
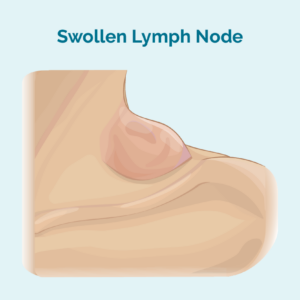
- Computed tomography (CT) scan – this is a common scan used to check the inside of your body. It can show if you have any swollen lymph nodes (lymphadenopathy), or if there are any tumours (collections of abnormal B-cells) in your body.
- Bone marrow biopsy – this test might be done to see if you have any monoclonal B-cells in your bone marrow.
Waiting for results
Waiting for results can be a difficult time. It may help to talk to your family, friends or a specialist nurse. You can also contact our lymphoma care nurses by clicking on the contact us button at the bottom of the screen.
Management of Monoclonal B-cell Lymphocytosis (MBL)
You do not need treatment for MBL. You will still have healthy B-cells to protect you from most infections and disease, and you will not have symptoms that make you unwell with MBL.
Your doctor will want to check your blood tests on a regular basis to make sure your lymphocyte count does not get higher. At first they may check every 3 months or so. If your lymphocyte count remains stable, you may only need a blood test once a year.
It is very rare for MBL to progress into CLL, but if it does it can picked up early through the regular blood tests. Even if you do develop CLL, you still may not need treatment. About 1 in 5 people with CLL never need treatment.
When to contact your doctor
You should contact your doctor if you start to experience any symptoms of lymphoma or CLL. These can include:
- Bruising or bleeding more than usual.
- Shortness of breath without reason.
- Extreme tiredness not improved with sleep or rest (fatigue).
- Infections that keep coming back or don’t go away.
- Itchy skin.
- A lump that come up under your skin caused by swollen lymph nodes (usually in your neck, armpit or groin).
- B-symptoms.
How to keep healthy living with MBL?
As well as increasing your risk of developing CLL, some research suggests that people with high count MBL may be at increased risk of other illnesses and cancers. This increased risk is not seen in people with low count MBL.
It is important to take care with your health and report and new or worsening symptoms to your doctor.
Below are some recommendations on living well with MBL.
- Protect your skin from sun exposure. When outdoors apply a SPF50+ sunscreen, cover your skin with clothes, wear a hat and sunglasses.
- Check your skin and report any new or concerning spots, rashes or wounds that don’t heal to your GP. It is also a good idea to have a yearly skin check with your GP or specialist skin cancer clinic.
- Have a blood test to check the level vitamin D. Your GP will tell you if you need to take vitamin D supplements.
- Keep up to date with any immunisations (vaccines) available to you. This includes the yearly influenza vaccine and recommended vaccines when travelling to other parts of the world. Live vaccines are not recommended for people with MBL. An example of a live vaccine is MMR (measles, mumps and rubella. Ensure you check this with your GP.
- Always attend age appropriate cancer screening checks including colonoscopy, mammogram and pap smears.
- Eat well, exercise and maintain a healthy weight. If you would like advice on this, ask your GP for a management plan that can include seeing a dietician, physiotherapist or exercise physiologist.
Summary
- MBL is not cancer, but can increase your risk of developing CLL or other types of cancer.
- MBL develops from a single abnormal cell that makes clones of itself.
- MBL can be low count or high count. High count MBL may progress to CLL, however this is very rare.
- MBL does not need treatment and does not cause symptoms, but you should have regular blood tests to check your lymphocyte count.
- Healthy living and having regular check-ups with your doctor is important when you have MBL.
- Report and new or worsening symptoms to your doctor.

