This is a picture of my Husband Ben and I, taken on the 28th of September 2022 at around 7:30pm. We were out celebrating my 30th birthday. We were also celebrating our one-month wedding anniversary. Three hours before this photo was taken, we also found out that I had two large masses growing in my chest, invading my sternum bone.
Rewind to a month before, Ben and I got married in Melbourne. I was not unwell on our wedding day; I had none of the symptoms that you would think someone with cancer would or should have. I was physically the fittest I had been in years.
After a week away for our mini honeymoon, we got home, and I flew straight to Sydney to start my new job. I had just landed my dream job as the head of HR transformation for a large, aged care and healthcare provider. My first two weeks involved lots of flying between Melbourne and Sydney and after my first week I was feeling tired, which I put down to getting up at 5am catching the red eye to Sydney, meeting new people, working and sleeping in a different place. I didn’t think anything sinister was going on.

Sarah and Ben celebrating her 30th birthday and their one month wedding anniversary
The start of my second week on that Monday, as I flew up to Sydney, I felt a pain in my chest. It was not a breathing pain, but more of a constant sharp piercing pain in my sternum. I figured I had pulled a muscle at Pilates, but the pain escalated through the week and when I got back to Melbourne I booked in to see my GP the following Wednesday.
My GP Elaine wasn’t convinced that it was just a pulled muscle and sent me off for urgent bloods to see if I had a blood clot from all the flying. At 6pm that night Elaine called me and said, “you have an elevated D dimer, I suspect this is a blood clot, you need a CT scan first thing tomorrow morning”. I wasn’t thrilled with this but at least we were getting closer to what was causing the chest pain.
I woke up on the morning of September 28th, it was a Thursday and the day of my 30th Birthday. By this stage I could only whisper because the vibration from my own vocal cords would cause me excruciating pain. I whispered “happy one month anniversary” to Ben and then asked him to drive me to my CT scan.
To be honest I was so in the zone at work that day I didn’t even think about the scan for the rest of the day. I was focussed on my first week in the Melbourne office, meeting new people and busy building my brand as “the weird new girl who whispers”. But at 4pm my phone rang, I recognised Elaine’s number and answered, “Hi Elaine, what am I dying from?” She said “Look, we are going to work through this, but your CT scan has shown two large masses in your chest. One the size of a small, sweet potato and the other a kiwi fruit. Both masses are pressing right up against your sternum bone. It’s most likely lymphoma, but we need to do a biopsy to confirm, do I have your permission to call an oncologist?” It was a life changing phone call, what you never expect to receive, especially not on your 30th birthday!

Ben with Sarah while she had her first CT Scan
Ben and I went out for Birthday dinner, parma and margs and at 7pm whilst at dinner my phone rang, an unknown number. I answered and it was my new oncologist Kirstin, she said “Happy Birthday Sarah, I’ve booked you in for tomorrow, see you then, we’ve got you”. That phone call at that moment was the most reassuring thing that had happened to me that day. And I thought, I wonder how many other people got an oncologist for their 30th birthday, that’s pretty unique!
The next day Ben and I met Kirstin, my oncologist from the Blood Unit at Cabrini Hospital in Malvern. She explained this was presenting as Hodgkin’s Lymphoma and that a PET staging scan was critical to determine where else the tumors were and assess what stage I was at. Kirsten talked through what treatment could look like without knowing the official diagnosis. We left that appointment with scripts for pain management, the staging PET scan booked, as well as two biopsies booked in. We left feeling a bit more comfortable with the situation.
So that next week I had the PET scan and then a few days later the biopsies. It was a hard time because as much as I wanted to not think about this 24/7, the pain in my chest, although manageable, was a constant reminder that something was happening and that it wasn’t good.
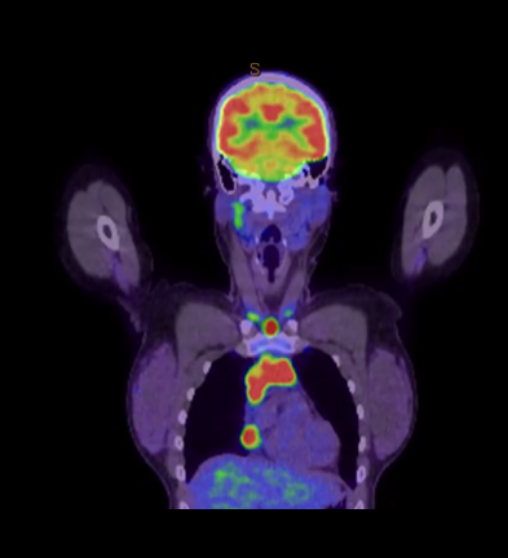
Sarah’s first PET Scan showing the tumours in her chest
Thursday the 13th of October, exactly two weeks since my CT scan, was the day we got the official diagnosis. Ben and I went to Cabrini and met with Dr Kirstin. She said, “It’s not bad news, it’s just not what we were expecting.” My diagnosis was Primary Mediastinal Diffuse Large B Cell lymphoma. A rare and aggressive form of non-Hodgkin’s lymphoma, I was stage 2E. This dramatically changed our treatment plan. Kirsten walked us through my regimen, DA R EPOCH and the concept of me getting day chemo was quickly replaced with inpatient immunotherapy and chemotherapy from Monday to Saturday on a 21-day cycle. Kirsten said, “I’ve booked you in for your PICC line, we are going to start chemo on Monday, Suzanne, one of our nurses is waiting for you now and she will answer any questions you have and talk you through fertility options”.
So, Ben and I sat down with Suzanne, and she said, “this is a lot, let’s just take a breath and I’ll walk you through what I have prepared, we’ve got you”. She explained this mythical PICC line, and she said I could expect to lose my hair quickly. I said to her, “I think Kirsten may have gotten me confused with another patient because she said something about fertility? My tumors are in my chest not my ovaries, what does lymphoma have to do with my fertility?”
I look back at this question and laugh because it’s now very obvious to me, but it goes to show that when you are new to cancer, everything is completely foreign. I was on a steep learning curve. We didn’t have time for egg freezing and after meeting with a fertility specialist the next day we started monthly injections in the hope to preserve my fertility.
By the end of the week, we had the facts, we had the plan. We had 48 hours to tell our friends and family before I started treatment. By Sunday night we were exhausted. I pulled out my work suitcase and instead of packing for Sydney, I started packing for my hospital stay. We were feeling as ready as anyone could be ahead of their first week of treatment.
Day one of treatment arrived, my PICC line was put in and my first cycle ran from Monday afternoon to Saturday morning. It didn’t take long for the nurses and wider medical team to work out that I was “that type of patient” and they started to keep me more informed with things that helped make me feel more comfortable and in control. It was the simple things like sharing the results when taking my blood pressure or temperature. Taking the extra second to say 36.8 was a win for me and made me feel more aware of my body. As a cancer patient you lose a lot of faith in your own body and knowing your own results, your own data, helps to bring back some of that lost control.
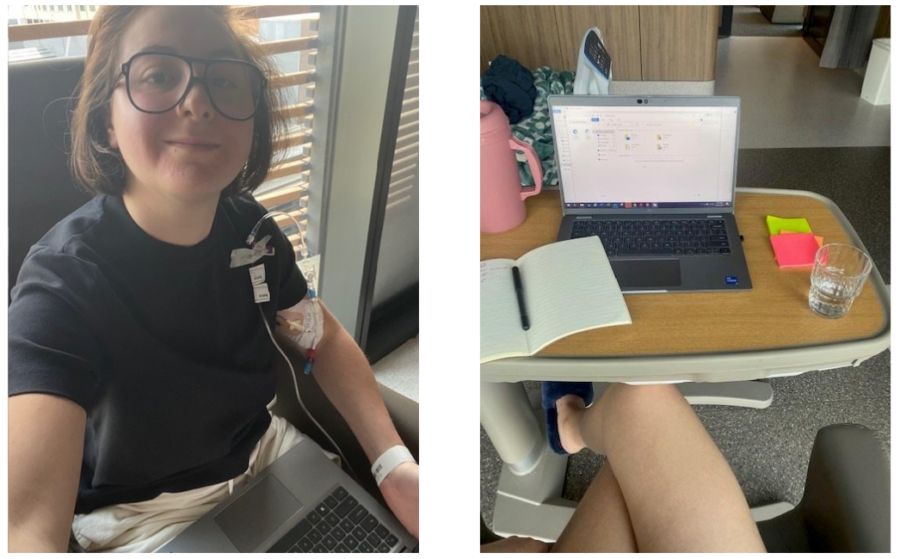
Sarah continued to work through her treatment with help from the nurses.
I decided to continue working throughout my treatment. The first morning I woke up in hospital I was feeling good. So, I set up my meal table as my desk, opened my laptop and started working. A squad of nurses came bustling in ready to take bloods, do observations, take my weight, etc. I remember looking up at everyone and I said, “well that’s not going to work, I have a meeting now!” Emily, one of the nurses, looked me up and down and laughed “you’re joining a meeting in that?” I completely forgot that I was in my snoopy donut nighty and was unable to get changed by myself due to my PICC line being connected.
Emily quickly got me changed, took the bloods and said she would pop back after my meeting for the rest. When she returned, she sat down and said “You’re here for treatment, it’s great you want to work but that must come second to why you are here. These are the non-negotiables and how we are going to make this work”. Morning bloods, any beeping from the chemo machine, bag change overs, and observations were the non-negotiables. And then she made a sign for my door when I was in any meetings.
The days went by slowly, but the weeks went quickly and before we knew it, we were at cycle three. I felt like I was mentally and physically in a good place. My chest pain had nearly gone, and I was no longer taking any pain medication.
So far, we had only told the small number of people who attended our wedding. It wasn’t like we were trying to hide it; we just didn’t really get around to telling everyone. So, what do you do in this day and age if you have a life update? You post it on Instagram! So, I did, I said “For my 30th birthday I got lymphoma”. I also announced I had made a separate account called Lymphomo where I would do a brain dump of things I was feeling for those who wanted to follow along. It was like a weight had been lifted off my shoulders. A weight that I didn’t even know was there. It felt good. I started to connect with other lymphomies and it’s how I met my now very good friend Chantelle. She had the exact same diagnosis as me, with the same treatment and was one month ahead. We spoke every day and became a pillar of support for each other.
But then the Instagram algorithm did its thing and I started seeing accounts of really sad and awful cancer experiences. People with the same cancer as me where the treatment didn’t work, widows, it was a lot. I had a lot of people reach out to share their stories and as much as I wanted to help I knew I couldn’t and I began to feel overwhelmed and consumed by it.

Announcing her diagnosis on Instagram
Going into cycle four I was in the worst headspace I had ever been in. The adrenaline had worn off, I just wanted it to be over. I had my halfway PET scan coming up and I couldn’t “unsee” those Instagram accounts where the treatment didn’t work. I was spiraling. One of my nurses, Maddy, noticed I was not my usual self, she re-opened the blinds in my room, and we watched the sunset together. She ended up staying 20 mins after her shift had finished to just chat and calm me down. I told her about the stories on Instagram and about my upcoming PET scan and she said something to me that has genuinely changed my outlook in life. She said, “You only ever hear about the planes that crash”. That story you hear in the news, that story you’re reading on Instagram, that is the plane that crashed. For every story you hear, you need to think about how many planes landed today. Think of all the good news stories that didn’t make it to the headlines, to your Instagram account. This piece of advice is something I have shared with nearly every cancer patient who has reached out to me. So not only has Maddy’s advice changed my experience but so many others in this fight. It’s a phrase my own friends have used back on me when I start to spiral.
Maddy’s advice got me through to the halfway pet scan. It was all looking much better, but we knew we were not out of the woods just yet. We shared the news with our inner circle and told them we were cautiously optimistic.
Cycle five was Christmas time and I got a very special gift – my very first blood transfusion. It set me up for a really good two weeks at home and I loved it so much that I was looking forward to getting another one for cycle six, knowing how great I felt afterwards.
When I was diagnosed with lymphoma in September last year, my stepdad Raoul was in his own battle with Acute Myeloid Leukemia after being diagnosed back in 2020. He reached remission, had a bone marrow transplant and unfortunately his leukemia returned with a T cell mutation.
Telling Mum and Raoul that I too had cancer was heart wrenching. He was on a clinical trial at the time, and I almost didn’t want to tell him. I knew this would tip him over the edge and I felt immensely guilty. Raoul started to decline rapidly and was admitted into hospital on the weekend of my first week back at home during cycle five. My neutrophils were 0.3 and going to visit him was not advised as he was sick and my immunity was low. But my medical team knew how important this was and told me to visit when no one else was there and to mask up. I went at 7am on a Sunday morning and sat with Raoul for hours. I said goodbye and I’ll see you tomorrow. Little did I know that was the last time I would ever see Raoul. He passed away the next day.
Attending your Dad’s funeral, when he has passed well before his time, is devastating. Attending your Dad’s funeral who has passed away from cancer when you too are a cancer patient is a feeling I really struggle to describe. It’s the opposite of surreal. It’s as real as it can get. It is the reality of what happens when your treatment doesn’t work. It was a really hard time for our family and selfishly, extra hard for me as I had convinced myself that my treatment too was not going to work.
But my medical team got me back into the headspace I needed to be in to get me through this final cycle. Raoul’s courage and strength through his own treatment is what motivated me to pull myself together and get through it. And I did it.

Sarah celebrating Chantelle’s 33rd birthday
Treatment was over and it was a waiting game until my PET scan in 8 weeks. When the results finally came back, I was in remission. This was a really special moment for both Ben and I and we are so grateful that this was our outcome. We know that so many people don’t get to hear this news and we felt very lucky. And then I remembered, I needed to tell Chantelle, the girl I had become friends with from Instagram. She had received her PET scan results the week before mine and unfortunately, she was not in remission and would need to start on a second line of treatment in the coming weeks. I went from being so happy to being in remission, to feeling sick to my stomach with survivor’s guilt. How on earth was I going to tell her that I was in remission.
But I told her and of course she was thrilled for me. I reassured her that this wouldn’t change our friendship, I wasn’t going anywhere, and I was here to get her through this. Chantelle started her second line of treatment at Peter Mac and I visited her. But boy the survivor’s guilt was real. Chantelle’s second line of treatment unfortunately didn’t work either, so plan C was Car T cell therapy and I continued to visit. Chantelle received her final results three weeks ago and she is “almost” in remission, they are confident she will be in the clear for her next scan in a couple of weeks.
So now you’re in remission, your hair starts to grow back, your cancer is behind you and everyone thinks you’re normal again, it’s like nothing ever happened right? Being in remission is the best feeling you can ever have, but there is no going back to your pre-cancer life. It takes a while to recover and find your “new normal” and I spent a lot of April and May in bed.
As time goes on, I am definitely feeling a little stronger every day and starting to socialize and actually go out to places. It is exciting to be able to resume some sort of normality and do everyday things again. But we are still learning our new normal.
I am back working in the Melbourne Office a couple days a week. And my next 6 monthly PET scan will be in September, as well as my “30th” birthday redo. If the PET scan results are not what we hope, we will be hitting up the pub anyway, but this time with a group of friends.
I’ve found that there is a lot of pressure on cancer patients to find a silver lining to their diagnosis. I would be lying to you if I said that it has completely changed my perspective. I would like to think that it has, and that I don’t stress the small things, but I still do, because I care.
So, if I had to find a silver lining it would be having the opportunity to raise awareness for blood donations and joining the donor registry. When I started my Lymphomo Instagram account I had no idea it would grow into a community of incredible people wanting to selflessly help others. This is something I will continue to raise awareness for.

Sarah in remission and finding her “new normal”
What advice would you give someone who has been recently diagnosed?
How has Lymphoma Australia helped you during your lymphoma journey?
Lymphoma Australia have been a safe space to talk about anything and everything. They have connected me to a community of people who have also experienced lymphoma. They have also been so helpful with recommending products to use for sensitive skin and things I didn’t even know I needed!
Sarah recently attended our 2023 Nurse Conference in Queensland to share her story with health professionals from across Australia.
She is now proudly sharing her story to help us shine a light on lymphoma this September for World Lymphoma Awareness Month.
We are so grateful to Sarah for giving us an insight into such an emotional and difficult time in her life. However learning about others experiences can be incredibly helpful and powerful for those on a similar journey.
If you would like to support our work in helping patients like Sarah, please consider donating today.
