What is Remission, Relapse and Refractory Lymphoma?
Remission
Complete remission is when your scans & tests show no sign of lymphoma in your body after treatment.
A partial remission is when there is still lymphoma in your body, but it is less than half of what it was before treatment.
Relapse
Refractory
Remission verses a cure
A cure is when you have no signs of lymphoma left in your body and it is not likely to return. Doctors often prefer to use the term remission, because we know lymphoma can come back.
The longer you are in remission the less likely it is for an aggressive lymphoma to come back, so your doctor may eventually say you are cured, but usually they will use the term remission. This is because while many people may never have their lymphoma come back, we don’t know exactly who will and who will not relapse.
Some people may have certain risk factors that make it more likely to come back, but you need to talk to your doctor about your own risk factors and chances for cure, remission or relapse.
What happens when lymphoma relapses?
Your doctor will continue to monitor you after you finish treatment, and one of the reasons they do this is to watch for signs and symptoms of your lymphoma relapsing. By continuing to see you regularly, they will be able to pick up any relapse early, and order more tests or start treatment again when needed.
Although it may be disheartening to find out your lymphoma has relapsed, it’s important to know that even relapsed lymphoma usually responds well to treatment, and may result in you going into remission again.
Relapses are very common in people with indolent lymphoma because indolent lymphomas are not considered curable. Instead, you will live with an indolent lymphoma for the rest of your life. However, in between treatments and during times of remission, many people live a normal life and many also have a normal life span.
In some rare cases, an indolent lymphoma may transform into a different, and more aggressive subtype of lymphoma. Transformed lymphoma is different to a relapse. To learn more about transformed lymphoma click the link below.
Why does lymphoma relapse?
Relapse can happen for several reasons. Some of these include:
- There is no known cure for some lymphomas, particularly indolent lymphomas. So, while the treatment is effective at managing the disease it cannot cure it. When you have indolent lymphoma, there will always be some lymphoma cells left that have the potential to wake up and grow.
- Some genetic mutations cannot be cured by current treatments. So, even if there is no sign of lymphoma left in your body, some genetic mutations may cause lymphoma to grow again.
- Even when scans and tests show there is no lymphoma left in your body, there can sometimes be microscopic lymphoma cells that are too few or small to be detected by current tests and scans. If these are present, they can grow and multiply after treatment ends.
How soon does a relapse happen?
If you have an aggressive lymphoma such as Hodgkin Lymphoma or a highly aggressive (fast growing) Non-Hodgkin Lymphoma, a cure is more likely. However if you do relapse, it would usually happen within a couple of years of treatment finishing.
If you have an indolent (slow growing) Non-Hodgkin Lymphoma, a relapse is more common. While a relapse can happen within months of finishing treatment, often remission lasts many years before a relapse.
Learn about treating relapsed lymphoma with Dr Michael Dickinson
Haematologist
How do you know if the lymphoma has relapsed?
Lymphoma may return in the same part of your body or it may affect a different part of your body from when you had the lymphoma before. You may or may not have symptoms and if you do, they may include:
- New or lymph nodes or lumps that are not related to an infection or illness
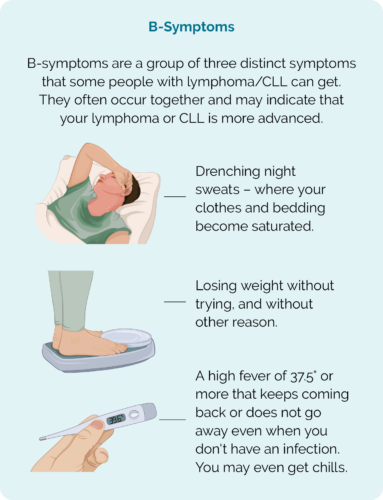
- Drenching night sweats
- Unexplained weight loss
- Fatigue that is worse than normal
- Itching
- Skin rash
- Diarrhoea
- Unexplained pain or discomfort
- B-symptoms.
What happens if lymphoma relapses
- Biopsy of new enlarged lymph nodes or lumps
- Blood tests
- Positron emission tomography (PET) scan
- Computed tomography (CT) scan
- Lumbar puncture if lymphoma is suspected in central nervous system.
What happens if my lymphoma is refractory to treatment?
It can be distressing to find out your current treatment is not working to cure, stop or slow down your lymphoma. Feeling scared, angry or anxious is quite normal. It is important to understand though, that just because this treatment didn’t work as planned, it does not mean hope is lost. Many lymphomas that don’t respond well to first-line treatment, can still have a good response to second or third-line treatments.
Refractory lymphoma can happen when the lymphoma cells develop safety barriers or checkpoints that make them immune to standard treatments. Certain genetic mutations can also make it less likely for some anti-cancer treatments to work effectively.
When this happens your doctor will want to try a different type of treatment that works in a different way to your current treatments.

How do I know if my lymphoma is refractory?
You will likely have scans after you’ve completed at least two or three cycles of your treatment. Exactly when you have these scans will depend on your individual circumstance, subtype and treatment type. Ask your doctor when you will have more scans and tests.
Usually after starting treatment you would notice that your swollen lymph nodes or other symptoms improve after a couple of cycles of treatment. However in some cases you may notice, or scans may show that the lymphoma has not improved and you may have new areas of lymphoma.
Your doctor may continue with your current treatment and do more scans after more cycles of treatment, or they may decide to change your treatment right away. They will talk to you about the best options for your individual circumstance.
Treatment options for relapsed or refractory lymphoma
The treatment options you are offered if you have a relapsed or refractory lymphoma will depend on many things, including:
- the subtype, stage and location/s of your lymphoma
- genetic mutations involved in your lymphoma
- if you have had a time of remission and if so, how long you were in remission
- your age and overall well-being
- how you have coped with previous treatments
- your eligibility for clinical trials
- your personal preferences.
Types of treatment for relapsed or refractory lymphoma
With clinical trials and new treatments being approved for treatment or management of lymphoma in Australia, we have more choices of second and third-line treatments than ever before. As such, because of the above factors, there is no one-size-fits-all approach to treatment. However, some of the treatments available in second and third-line treatment include:
- Clinical trial participation
- Combination chemotherapy
- Salvage chemotherapy (high dose chemotherapy)
- Stem cell transplant (autologous & allogeneic)
- Targeted therapy
- Immunotherapy
- Biological medicines
- Radiotherapy
- Chimeric antigen receptor (CAR) T-cell therapy
- Off label access to medications.
Off label access to medication
Sometimes, you might be able to access medications that aren’t publicly funded, but are declared safe and legal for use in Australia by the Therapeutic Goods Administration (TGA).
Important things to be aware of:
- This may not be an option for everyone as each state has different rules and regulations.
- You may need to travel for some or all of the treatment.
- It can be very expensive as you need to self-fund, or pay for it yourself. So, it is something that needs to be carefully considered and discussed with your haematologist to fully understand.
- In some cases, you may be able to access the medication on “compassionate grounds” where the pharmaceutical company pays for some or all of the cost of an off-label medication. Ask your doctor if this is an option for you.
Getting a second opinion
It is quite common for patients to ask for a second opinion. This is a good option to hear the thoughts of a second haematologist who may be able to confirm the information given to you by your first haematologist, or offer different options. There is no reason to feel bad about asking for a second opinion. Most haematologists are comfortable with you seeking a second opinion – It is your health after all.
If you would like to get a second opinion talk to your haematologist. Often, they can organise something for you, or you can talk to your GP. This is an important step in making sure you get the information you need to get the right treatment for your individual circumstances.
Learn more about 'off label access' in the video below
Planning for treatment
Dealing with the emotional and physical pressures of having lymphoma, and treatment can be exhausting. It is important to reach out and get support when you need it. Often we have people in our lives that want to help, but don’t quite know how. Some people also worry about talking about how you are going because they are concerned they will say the wrong thing, overstep or upset you. This does not mean they don’t care.
It can help to let people know what you need. By being clear about what you need, you can get the help and support you need, and your loved ones can have the joy of being able to help you in a meaningful way. There are some organisations that have put together plans you can use to coordinate some of the care. You may like to try:
Advance care planning
Advance care planning is a great way to make sure your medical team and family know what treatment you do, and do not want to have in the future.
Everyone should have an advance care plan. The forms needed and process for developing an advance care plan may differ from state to state. For more information on advanced care planning, and to access the right forms for your state, click the link below.
Palliative care
Many people think palliative care is about end-of-life care. While this is one of the roles, they also have another major role. They also help to manage symptoms and side-effects that are difficult to treat that you may experience at any point during your lymphoma. The main aim is helping to ensure you have the best quality of life during your treatment as well as at end of life.
Symptom/side-effect management
Lymphoma and its treatments can cause a variety of symptoms and side-effects. While your haematologist or oncologist can help with many of these, sometimes symptoms or side-effects need more specialised management. The palliative care team are experts at managing these. They also have access to medications that your haematologist or oncologist are not authorised to prescribe. The palliative care team are a great resource to improve your quality of life.
Some symptoms or side-effects they can help you manage include:
- pain – including peripheral neuropathy
- nausea with or without vomiting
- anxiety
- shortness of breath
End of life care
Successful clinical trials, means that there are a lot of new treatments that have significantly improved outcomes for people with lymphoma – even relapsed and refractory lymphoma. Many people live a long and relatively healthy life even after a lymphoma diagnosis. Unfortunately though, sometimes people die from lymphoma.
The most commonly understood role of palliative care is to help people who are nearing the end of their life to have control over how they live the rest of their life. They are fantastic at empowering you to think about, and plan your needs and where you would like to spend your time, whilst ensuring you are safe, with good quality of life during this time.
Support when you’re nearing the end of your life
Palliative care can also help your family and loved ones understand what is happening, and ensure they have the support they need during this time too. Other things they can help with include:
- organising equipment for you to use at home if you choose to stay home
- talking to loved ones about sensitive issues such as your end of life and funeral plans
- link you to different services in the community
- ensure your cultural and spiritual beliefs are upheld in your death
- counselling and emotional support.
Summary
- A cure is when there is no lymphoma left in your body and it does not come back.
- Remission can be complete or partial resulting no signs of lymphoma in your body (complete), or when the lymphoma cells have reduced by more than half (partial).
- Lymphoma can relapse (come back) after a time of remission. Remission can last weeks, months or many years.
- When aggressive lymphomas relapse, its usually in the first couple of years after finishing treatment. The longer you are in remission, the greater the chance of cure.
- Indolent lymphomas often relapse, but also usually respond well to treatments. You will live with an indolent lymphoma for the rest of your life, but can live well during times of remission.
- In some cases, lymphoma does not get better with first-line treatment – this is called refractory.
- Refractory lymphoma can still respond well to second and third line treatments.
- Advance care planning is important to ensure your family and doctors know wishes regarding your health care.
- Palliative care can help with symptoms and side-effect management.
- Some people will need end-of-life care if their lymphoma does not respond to treatments. Palliative care can be a great support, and ensure you have the best quality of life during the end-of-life time, and provide needed support to your loved ones.

