Trav is Hallam’s Journey with Hodgkin Lymphoma: Staying Strong in Mindset
is Hallam’s Journey with Hodgkin Lymphoma: Staying Strong in Mindset
The First Signs
“It’s hard to pinpoint exactly when it began,” Travis reflects. In early March 2025, he started experiencing “quite debilitating and unbearable symptoms”, severe pain in his shoulder blade, neck, jaw, headaches, and back. The discomfort quickly escalated into nerve pain down his right arm and sleepless nights, leaving him utterly exhausted. Despite countless specialist appointments, scans, tests, and medications, the pain simply would not ease.
As time passed, the symptoms worsened. Travis began struggling to breathe, and his neck and jugular vein swelled. This led to a CT scan that finally revealed “multiple swollen lymph nodes.” An urgent follow-up CT scan with contrast on his chest prompted a call within 1.25 hours, instructing him to return to his GP immediately and to bring his mother. “I had never thought there was anything wrong with my chest,” he admits, despite some minor tenderness around the collarbone.
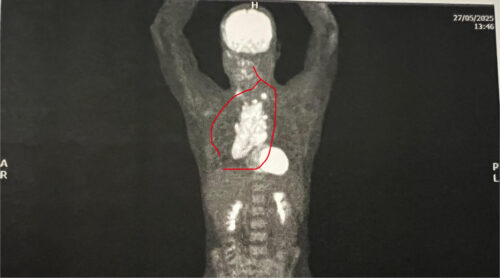
The following day, 22nd May 2025, Travis and his mother met with his GP. It was then that he learned about the mass growing in his chest: “It was explained that it was indicative and highly probable to be Lymphoma or some other form of cancer.” That same day, Travis was supported and triaged through the emergency department at Box Hill Hospital and the following day admitted into the cancer ward where a biopsy confirmed Classical Hodgkin Lymphoma Stage 2b. Travis remained at the ward for 2 weeks. The size of his ‘bulky disease’ was 14cm x 8cm x 6cm.
 Recognising the Symptoms
Recognising the Symptoms
Before his diagnosis, Travis’s symptoms were both disruptive and puzzling. “It started with severe shoulder blade pain on my right-hand side, then neck pain, jaw pain, headaches and back pain,” he recalls. “Eventually it progressed into nerve pain down my right arm and the inability to sleep, causing fatigue.” Despite seeing multiple specialists, undergoing scans, and trying various medications, nothing seemed to help. Over time, the pain worsened, and new symptoms appeared, shortness of breath, swelling around his jugular vein, and neck swelling.
When doctors began asking about typical lymphoma symptoms, more pieces of the puzzle fell into place. Travis realised he had also been experiencing subtle signs that he hadn’t connected to lymphoma. “Unexplained weight loss, for example I had put that down to my ADHD medication reducing my appetite, or to my chronic ulcerative colitis and the medications I was taking during a flare-up. Stress also seemed like a likely cause. But in hindsight, it was apparent that I was also experiencing lymphoma-related weight loss.”
Travis is clear that his ulcerative colitis flare-ups were a separate condition, not caused by lymphoma, but they added to the confusion in the early stages when doctors were trying to piece everything together.
Night sweats were another symptom that went unnoticed. “I sleep with a fan on and I often just run hot,” he explains. “So I assumed I just needed to turn the fan up. Absolutely caught me off guard that this too was a symptom of my lymphoma.”
Once treatment began his pain reduced quickly with strong pain management. Fatigue became the main lingering symptom, and the challenges he faced from that point were largely side effects of the treatment itself.
Treatment and Side Effects
Travis underwent escalated BEACOPP chemotherapy and, at the time of sharing his story, was on his fourth cycle, hopefully his last. “The response to treatment has been extremely positive,” he says, though fatigue remains persistent, particularly in the mornings and evenings, or after exerting himself. Constipation and nausea were occasional side effects, and the first cycle was especially challenging:
- Day 1: “Very unwell and nauseas, dizzy, tired, and as though I was going to pass out or throw up. I was in hospital for the first three days.”
- Day 2: “A bit more of the pain in my back/shoulder returned… treated with an increase in pain meds.”
- Day 3: “Simply very tired, fatigued and needed much more sleep.”
- Day 8: Fever-like shivers, eased with Panadol.
Subsequent cycles were milder, though fatigue remained the primary challenge.
Accessing Treatment
Fortunately, Travis did not have to travel far. He started as an in-patient due to the size of his mass, then continued as an out-patient with support from his mother and best friend, Sarah. “I was quite blessed and fortunate,” he says, noting that hospital-in-the-home visits helped monitor his PICC line and bloods twice a week.
Emotional, Mental, and Financial Challenges
Travis describes the emotional impact as immense: “Words such as ‘isolation, loss of autonomy/independence, fear’… have been difficult to navigate.” The whirlwind of diagnosis, hospitalisation, and treatment left him struggling to process his emotions. “The day I got home from the hospital, I jumped into the shower, turned it on hot, turned up the music and prepared to just let it all out and cry… Within two minutes, I ended up singing and just couldn’t cry.”
Mental health support, he observes, is not easily accessible: “Despite the 10 rebated sessions under the mental health care plan, I worry for those who may have more than just cancer happen to them.” He stresses the importance of protecting one’s mindset and accessing professional support where possible.
Financially, being a sole trader meant a substantial loss of income, around 10–12 weeks of wages, and a reduction in workload from six days to 2.5 days a week. Government benefits were limited or unsuitable, creating a significant burden. Physically, Travis faced hair loss, weight fluctuations, fatigue, and the ongoing presence of his PICC line. He takes a measured, “hour by hour, day by day, week by week” approach to try and reduce stress and worry.
Finding Strength and Routine
From day one, Travis focused on mental resilience. “Mind of Matter. Protect your mental health, Travis!” became his mantra. He relied on close family, friends, and the wider community for support, and found purpose in raising awareness and advocating for mental health supports.
Small daily practices such as mindfulness walks, affirmations, singing, gratitude, and staying connected were crucial. He also set up a comfortable living space for visitors, managed his medications efficiently with the local chemist, and maintained clear communications to preserve his energy. “Nothing worse than constantly feeling like your independence and decision making is getting less and less. Be vocal but be considerate.”
Discovering Lymphoma Australia
Travis had no knowledge of Lymphoma or available support before his diagnosis. Through Box Hill Public Hospital, he discovered Lymphoma Australia and began using their resources, received the patient treatment pack, accessed webinars, online support groups, and Facebook support groups. “I found a lot of strength and connection in the other champions/fighters… who just ‘get it.’ It’s SO powerful.”
Advice for Others
Reflecting on his experience, Travis shares:
- “Keep your mindset strong and access mental health support as quickly as practical.”
- “Encourage carers to access support too; they have their own journey alongside you.”
- “Stay connected to family, friends, and health professionals to prevent isolation.”
- “Listen to specialists, access reliable information, and protect your headspace. Mind over matter!”
He emphasises focusing on the present, embracing small blessings, and allowing oneself to be vulnerable, emotional, and, when necessary, selfish in a healthy way.
The Journey Ahead
Travis candidly admits that processing the emotional impact is ongoing. “Cancer came into my life, crashing down every wall… and now it’s about abruptly handing back 80% of my life.” He is learning to find his new ‘norm’, or as he calls it, his new ‘weird’, and is approaching life with gratitude, resilience, and a renewed appreciation for the moment. Through advocacy, fundraising, and sharing his story, Travis has transformed his journey into one of purpose and connection.
“I have CHOSEN to be happy, I have CHOSEN to not allow myself to think of the ‘what ifs,’ and I have CHOSEN not to focus on what I cannot control; instead, I focus on what I can.”