The CAR T-cell process
CAR T-cell therapy is a special treatment that helps your own immune system fight cancer. It uses a type of white blood cell called a T-cell lymphocyte. These cells are taken from your body, changed in a lab to help them better fight cancer, and then returned to you. This process takes time and planning, but it can offer hope to people with some types of blood cancer – including some B-cell lymphomas.
It can take up to 6 weeks between deciding to have CAR T-cell therapy and actually getting the treatment. This is because there are a lot of steps to getting this personalised treatment.
Because of this, your doctor will need to do tests to make sure it’s safe to wait for treatment. The lymphoma will need to be stable – meaning that it cannot be actively and quickly growing. If it is, you may need to start a different treatment sooner. If this is the case for you, you may not be able to have CAR T-cell therapy.
However, in some cases, you may be able to have a “bridging treatment”. This means having treatment with chemotherapy or other medicine while waiting for CAR T-cells. The aim of the bridging treatment is to keep your lymphoma stable and stop it from getting worse.
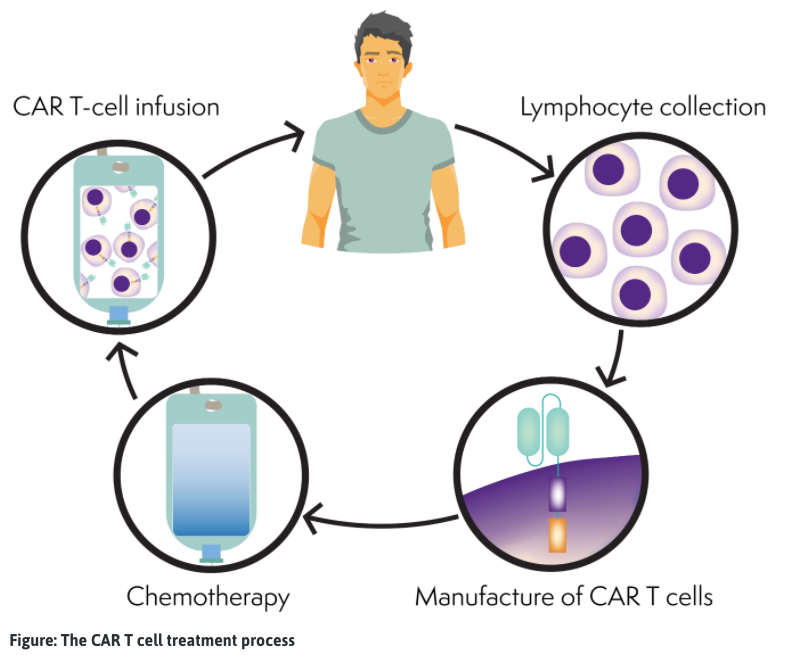
What’s the CAR T-cell process?
The CAR T-cell process is complex and you will have support from many health professionals during this time. Below is a step-by-step guide of what to expect.
1. Checking if You Can Have the Treatment (Eligibility Screening)
First, your doctors will do tests to see if CAR T-cell therapy is right for you. This includes blood tests, scans, and checking your overall health. If the tests show you’re a good match, the treatment process can begin.
2. Collecting Your T-Cells
Once you’re approved, your T-cells need to be collected. This happens through a procedure called apheresis. You will be connected to the apheresis machine with a tube running from your cannula or central line to the machine. The machine then gently and slowly pulls out some of your blood, processes it and takes out the T-cells. It then returns the rest of your blood back into your body.
To keep you safe, only a small amount of blood is removed at any time. This collection is done in a hospital or special clinic and can take several hours. You will be awake for this procedure, and it should not hurt at all.
3. Making T-Cells into CAR T-cells
After collection, your T-cells are sent to a special lab. There, scientists add a new part called a “Chimeric Antigen Receptor” (CAR). CARs help the T-cells find and kill lymphoma more effectively. This part of the process can take a few weeks.
The CAR is a special man-made protein. You can think of it as a special magnetic key that is attracted to, and locks onto lymphoma cells. Because the CAR is attached to the T-cell, it brings the T-cell straight to the lymphoma cell so it can fight and recruit other immune cells to destroy the lymphoma.
4. Getting Ready for the T-Cells to Return
Before you have your CAR T-cell infusion, you may need to have a short round of chemotherapy. This helps make space in your body so the CAR T-cells can multiply (make more CAR T-cells) and work better.
5. CAR T-Cell Infusion (Getting Your Cells Back)
Your modified T-cells – now called CAR T-cells are sent back to the hospital. You’ll receive them through a drip into your vein, like a blood transfusion. This is usually a simple and quick transfusion and often takes less than 30 minutes.
Once inside your body, the CAR T-cells go to work finding and fighting the lymphoma. They are also able to clone themselves. This means that they can make more copies of themselves, so you have even more CAR T-cells to fight the lymphoma.
6. Staying Close to the Hospital
After the infusion, you’ll need to stay in hospital for at least one to two weeks. This is to make sure your body reacts safely. Some side-effects are delayed, so even if you are well enough to leave hospital, you will need to stay near the hospital with your carer for up to 4-8 weeks. It’s important to have someone with you (a carer), as you may need help and support during this time.
Note: You are not allowed to drive for 8 weeks after CAR T-cell therapy, so it is important to have someone help you even after you are discharged from hospital.
If You Live Far Away
If you live in a rural or remote area, or a different state, you may have to travel a long way to get treatment. This can mean being away from your home, family, friends, work, pets, and other supports. Most people bring one main carer with them. This can be hard on families, especially if children or others are left behind.
Support from a Social Worker
During this time, a hospital social worker can help. They’re there to support you and your carer. They can help with travel plans, finding places to stay, linking you with financial support, and talking through any worries you have.
CAR T-cell therapy is a big journey, but you’ll have a health care team, including nurses, doctors, and social workers, to guide you every step of the way.
When children are affected by lymphoma
Children can be affected by lymphoma if they are the patient, or if a parent, brother or sister has lymphoma. This can be a scary time for them and forces them to face big stressors when they should be living care-free.
CAR T-cell therapy may also mean they are away from their parents or siblings for long times, which can be difficult – especially if you have to travel long distances for treatment.
There is support available for children and their families affected by lymphoma. Some organisations who can help include:

