What does indolent mean?
Indolent refers to how your lymphoma cells behave and grow. They are usually slow-growing with lymphoma developing over many months, or even years before being diagnosed. Because of the slow-growing nature of these lymphomas, you may not have any symptoms, and only be diagnosed with the lymphoma after having tests or scans for some other reason.
Indolent lymphomas also tend to go through stages, where they grow slowly for a while, sometimes they sleep and don’t do anything at all. But then they can ‘wake up’, and when they do, you may need to start anti-cancer treatment. When not having treatment, you will still be actively monitored by your specialist doctor. This is often called Watch & Wait and is when the doctor continues to watch the progress of your lymphoma, to make sure it is not growing, or causing you signs or symptoms that may need treatment.
For more information on Watch & Wait click the download button below.
Are indolent lymphomas curable?
Most indolent lymphomas are considered chronic diseases that you will live with for the rest of life. They are usually not curable, but many people can still live a normal life-span and a good quality life with it. Having treatment for indolent lymphoma is usually to either manage symptoms, or to put the lymphoma into complete or partial remission. However, it is very rare for an indolent lymphoma to be cured.
What's the difference between a cure and remission?
Scroll over the boxes below to learn the difference between a cure and complete or partial remission.
Cure
Complete remission
Partial remission
What happens when indolent lymphoma's relapse, or do not respond to treatment
It is common and somewhat expected, for indolent lymphomas to relapse after a time of remission. When this happens you will need to have more tests and biopsies. Once the results of these are in you will likely be offered more treatment with the aim to put you into remission again.
We don’t know exactly how long people will stay in remission for. Some people only ever have treatment once and never need it again, while others may relapse after a few months, and others after many years.
If your indolent lymphoma does not respond to treatment it is called refractory. Refractory lymphomas are resistant to some treatments but may respond well to different types of treatment. If your lymphoma is refractory, your oncologist or haematologist may want to start you on a different type of treatment that may be more effective for you.
What does it mean if my indolent lymphoma transforms?
In some cases, an indolent lymphoma may develop new genetic mutations and transform – or change into a different, more aggressive subtype of lymphoma. When this happens, you will need treatment for the more aggressive subtype of lymphoma. For more information on transformed lymphoma, click the link below.
When should I see my doctor?
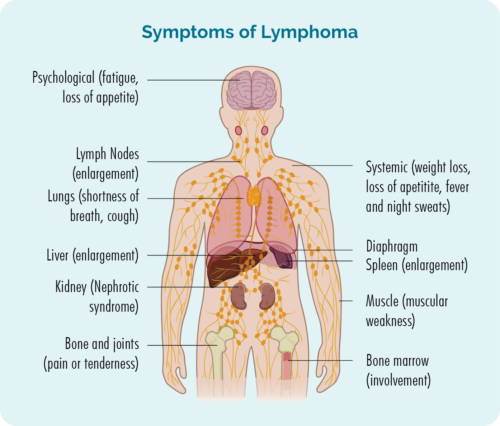
You will continue to be actively monitored by your specialist doctor even when you are on Watch & Wait and in remission. It is important that you report and new or worsening symptoms to them. If you notice you are getting the symptoms in between your specialist appointment, contact your specialist team and ask for advice. Some symptoms to report immediately include:
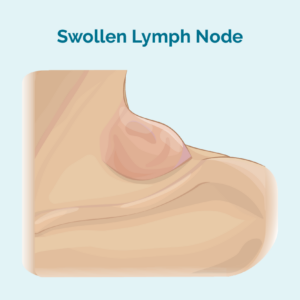
- A growing lump, particularly in your neck, armpit or groin (swollen lymph node).
- New or worsening pain, difficulty breathing or changes to your voice.
- Ongoing fatigue (extreme tiredness) that does not improve with rest or sleep.
- A rash or itch that does not go away.
- Unusual bleeding or bruising.
- Infections that do not go away or keep coming back.
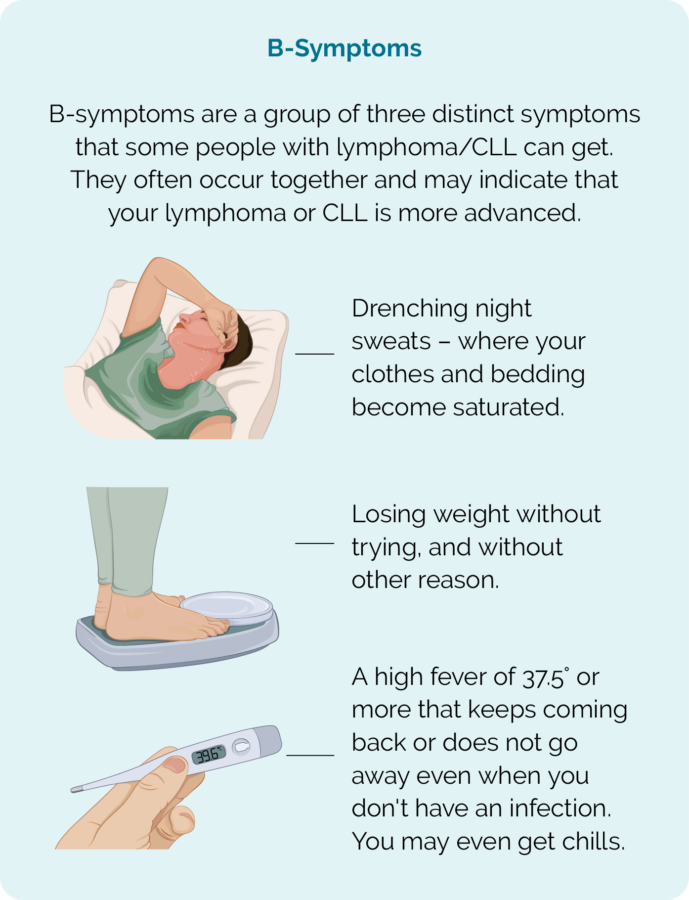
- B-symptoms.
Summary
- Indolent lymphomas are slow-growing cancers of white blood cells called lymphocytes.
- You will likely live with your indolent lymphoma for the rest of your life, and may go through periods of watch and wait and times of treatment.
- Many people have good quality of life even with indolent lymphoma, and many also have a normal life-span.
- The aim of treatment for indolent lymphomas is to improve symptoms, or put you into remission, but it is common for indolent lymphoma to relapse and need more treatment.
- In some cases, your indolent lymphoma may begin to act more aggressively, or even transform into an aggressive subtype of lymphoma. Transformed lymphoma is treated in the same way the aggressive lymphoma is usually treated.
- Let your doctor know if you have any new or worsening symptoms as listed above.
- Contact our lymphoma care nurses by clicking on the “Contact Us” button at the bottom of this page.