Overview of Transformed Lymphoma (TL)
Transformed lymphoma happens when your indolent lymphoma changes, and becomes an aggressive lymphoma with features of a different subtype of lymphoma. This is different to your indolent lymphoma “waking up” or becoming more active and needing treatment. In some cases, you may have both indolent and aggressive lymphoma cells as the lymphoma goes through the process of transforming.
Indolent lymphomas are typically made up of small, slow growing cells. However, if many of these cells start growing bigger, and quickly, the lymphoma begins to act like an aggressive lymphoma such as Diffuse Large B-cell Lymphoma (DLBCL). It is not uncommon when you have a transformed lymphoma, to have mixed lymphoma cells, some that are indolent and others aggressive.
Aims of treatment for your indolent or transformed lymphoma
Most indolent lymphomas will go through stages where they sleep and wake up. However, if your indolent lymphoma becomes more active and needs treatment, you will have treatments directed at managing your indolent lymphoma.
However, if your indolent lymphoma transforms into an aggressive subtype of lymphoma, you will likely have treatment directed at curing, or putting the aggressive lymphoma into remission.
Why does transformation happen?
Lymphoma can transform when the lymphoma cells, or the genes that provide instructions to your cells develop new genetic mutations. These new mutations can be a result of previous anti-cancer treatment, or can happen without a known cause. The genetic changes can alter the way the lymphoma develops and behaves, resulting in a more aggressive nature.
Who is affected by Transformed Lymphoma?
Anyone with a low-grade lymphoma or indolent lymphoma is at risk of a transformation. However it is very rare, and only happens in about 1 to 3 people in every 100 with indolent lymphoma each year (1-3%).
You will have a slightly higher risk of a transformation if you have bulky disease (a large tumour or tumours) when you are first diagnosed with your indolent lymphoma.
The most common indolent lymphomas that can transform include B-cell lymphoma such as:
- Follicular Lymphoma
- Chronic Lymphocytic Leukaemia or Small Cell Lymphoma
- Marginal Zone Lymphoma
- Nodular Lymphocyte Predominant B-cell Lymphoma (previously called Nodular Lymphocyte Predominant Hodgkin Lymphoma)
- An indolent Mantle Cell Lymphoma
- Waldenstrom’s Macroglobulinemia
It is important to understand that most people with these lymphomas do not transform.
Some people with an indolent T-cell lymphoma may also have a transformation, but these are even rarer.
When is a transformation most likely to happen?
Transformed lymphoma can happen at any time, but you are most likely to have a transformation about 3-6 years after you are diagnosed with your indolent lymphoma.
The risk of a transformation decreases significantly after living with your indolent lymphoma for 15 years, with transformations after this time being very very rare.
Symptoms that may indicate your lymphoma has transformed
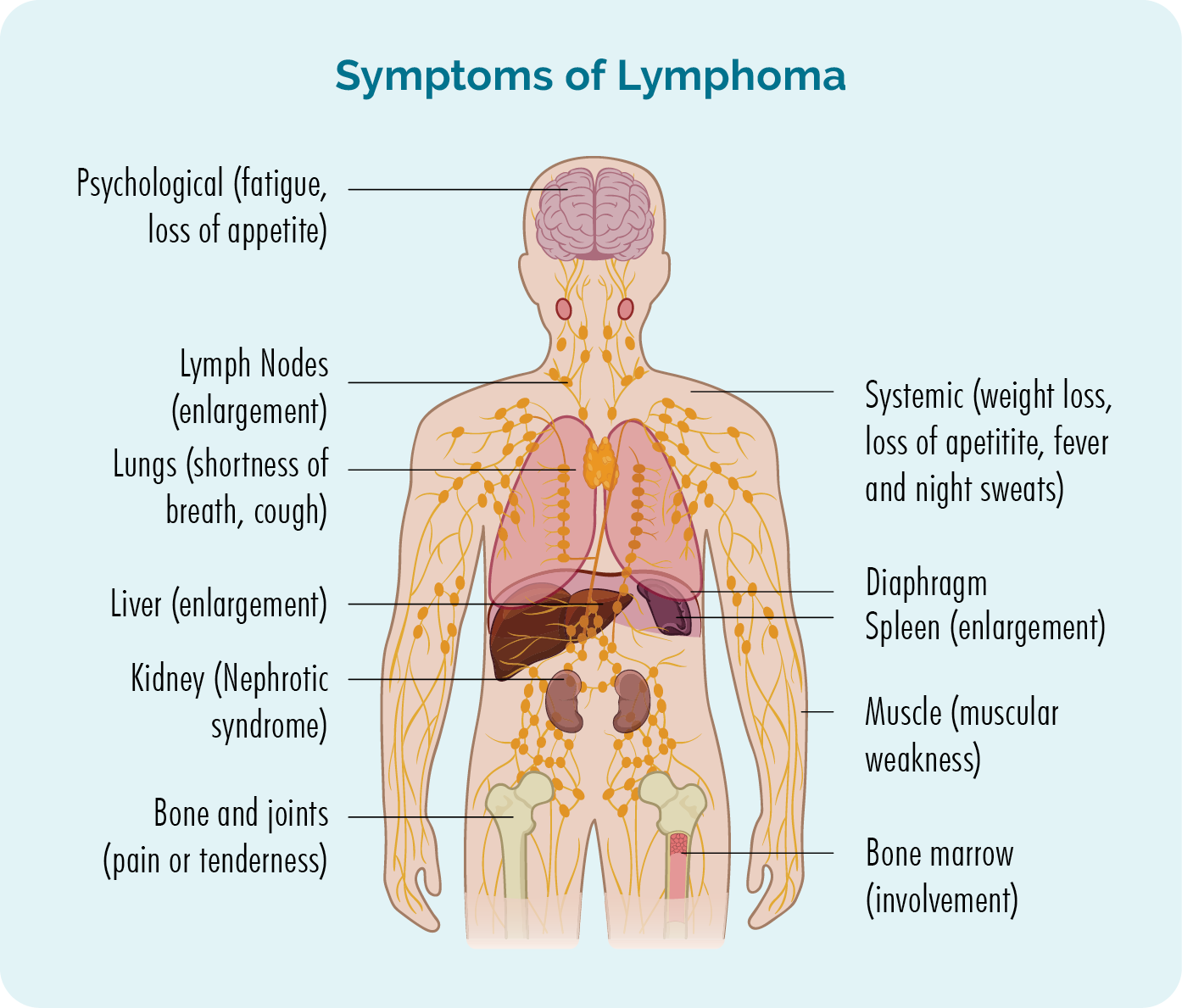
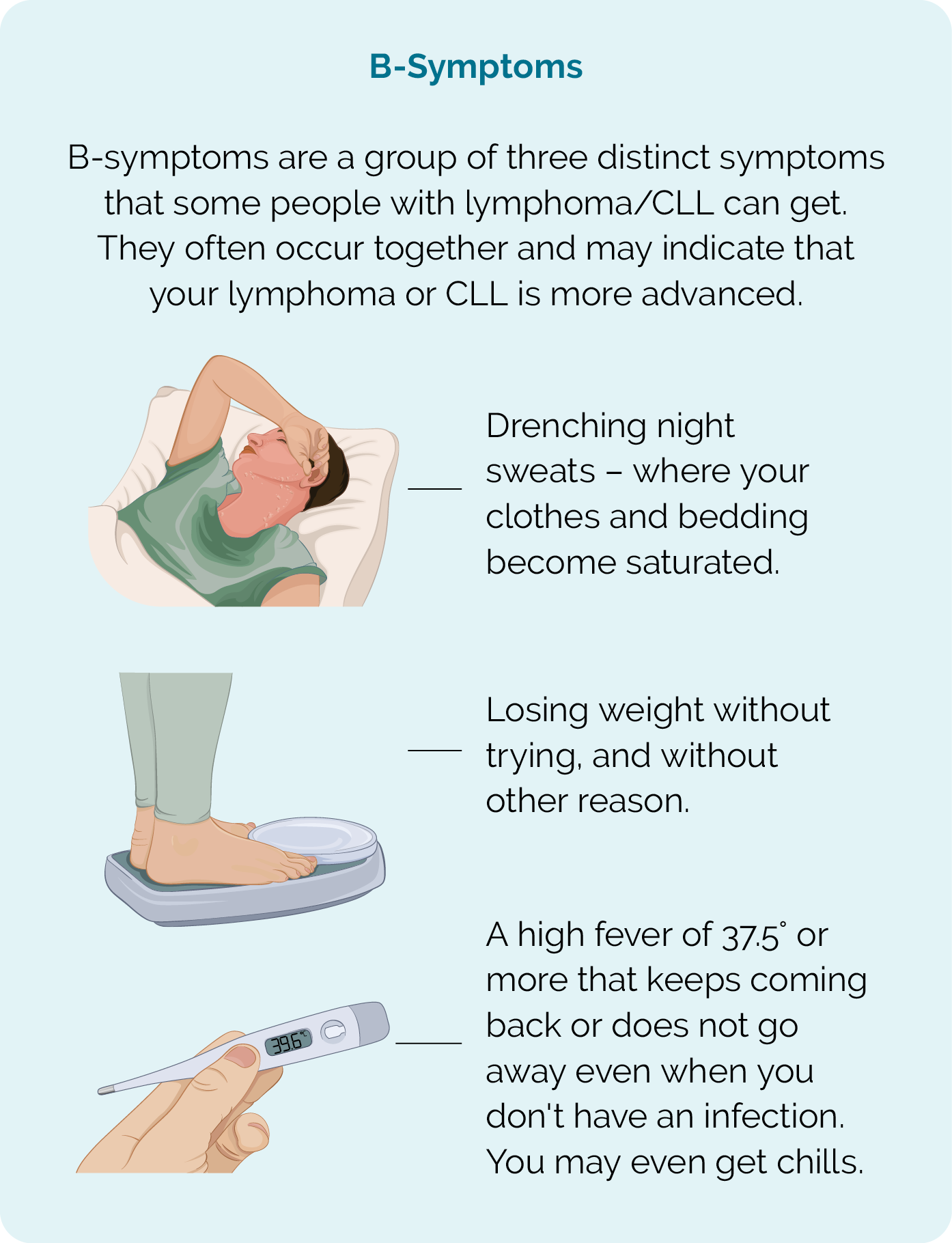
You may also get B-symptoms as your lymphoma becomes more active or begins to transform
What are the most common transformations?
Some transformations are more common that others. Below we list the more common (though still rare) transformations that can happen.
Indolent lymphoma |
Can transform into the following lymphoma |
| Chronic Lymphocytic Leukaemia/Small Lymphocytic Lymphoma (CLL/SLL) |
Transforms to Diffuse Large B-cell Lymphoma (DLBCL) – this transformation is called Richter syndrome. Much more rarely, CLL/SLL can transform into a classical subtype of Hodgkin Lymphoma. |
| Follicular Lymphoma |
Most common transformation is to Diffuse Large B-cell Lymphoma (DLBCL). More rarely, can transform into an aggressive B-cell lymphoma, with features of both DLBCL and Burkitt Lymphoma. |
| Lymphoplasmacytic Lymphoma (also called Waldenstrom’s macroglobulinemia) | Diffuse Large B-cell Lymphoma (DLBCL). |
| Mantle Cell Lymphoma (MCL) | Blastic (or blastoid) MCL. |
| Marginal Zone Lymphomas (MZL) | Diffuse Large B-cell Lymphoma (DLBCL). |
| Mucosa-Associated Lymphoid Tissue Lymphoma (MALT), a subtype of MZL | Diffuse Large B-cell Lymphoma (DLBCL). |
| Nodular Lymphocyte-Predominant B-cell Lymphoma (formerly called Nodular Lymphocyte-Predominant Hodgkin lymphoma) | Diffuse Large B-cell Lmphoma (DLBCL). |
| Cutaneous T-cell Lymphoma (CTCL) | Large Cell Lymphoma. |
Diagnosis and staging of Transformed Lymphoma
If your doctor suspects your lymphoma has transformed they will want to do more tests and scans. The tests will include biopsies to check if the lymphoma cells have developed new mutations, and if they are now behaving more like a different subtype of lymphoma, and scans will be to stage the lymphoma.
These tests and scans will be similar to the ones you had when you were first diagnosed with lymphoma. The information from these will give your doctor the information needed to offer you the best type of treatment for your transformed lymphoma.
Treatment
Once all of your results from the biopsy and staging scans have been completed, your doctor will review them to decide the best possible treatment for you. Your doctor may also meet with a team of other specialists to discuss the best treatment and this is called a multidisciplinary team (MDT) meeting.
Your doctor will consider many factors about your lymphoma and your general health to decide if, and what treatment is needed. Some of the things they will consider include:
- What transformation has happened (your new subtype of lymphoma)
- The stage of the lymphoma
- Any symptoms you are getting
- How the lymphoma is affecting your body
- Your age
- Any other medical problems you have or medications you are taking
- Your preferences once you get all the information you need.
Types of Treatment
Transformed lymphoma needs to be treated in the same way as an aggressive lymphoma. Treatment can include:
- Combination chemotherapy
- Monoclonal antibody
- Autologous stem cell transplant (if healthy enough)
- Radiotherapy (usually with chemotherapy)
- CAR T-cell therapy (Chimeric antigen receptor T-cell therapy – after 2 prior therapies)
- Immunotherapy
- Targeted therapies
- Clinical trial participation
Prognosis of Transformed Lymphoma (TL)
Many aggressive lymphomas can be cured, or have long times of remission after treatment. As such, there is hope that when given treatment you may be cured, or have a long lasting remission from the more aggressive, transformed lymphoma. However, you will still need close follow-up after your treatment to check for signs of relapse.
Indolent lymphomas in most cases cannot be cured, so even after the treatment for your transformed lymphoma, you may still have some indolent lymphoma cells left, and as such your doctor will want to check this too.
Ask your doctor what chances you have of being cured, going into remission and still living with indolent lymphoma after treatment for your transformed lymphoma.
Summary
- Transformed lymphoma is very rare, with only about 1-3 out of every 100 people with an indolent lymphoma having a transformation each year.
- Transformed is more common in people with an indolent B-cell lymphoma, but can happen in people with an indolent T-cell lymphoma too.
- Transformation is more common 3-6 years after you are diagnosed with an indolent lymphoma, and very very rare after 15 years.
- Transformed Lymphoma can happen if your genes or lymphoma cells develop new mutations, changing the way the lymphoma grows and behaves.
- Transformed Lymphoma is different to an indolent lymphoma “waking up” and becoming more active.
- There is still potential to be cured from the more aggressive transformed lymphoma, but you may continue to live with the indolent lymphoma after treatment.
- Treatment for transformed lymphoma will be targeted at curing, or putting the aggressive lymphoma into remission.
- Report all new and worsening symptoms, including B-symptoms to your doctor.

