Overview of cutaneous (skin) lymphoma
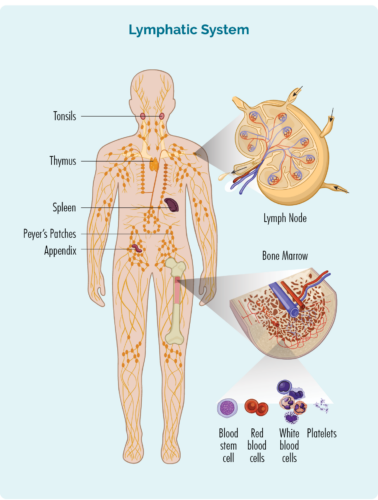
Lymphoma is a type of cancer that starts in white blood cells called lymphocytes. These blood cells usually live in our lymphatic system, but are able to travel to any part of our body. They are important cells of our immune system, fighting infection and disease, and helping other immune cells work more effectively.
About Lymphocytes
We have different types of lymphocytes, with the main groups being B-cell lymphocytes and T-cell lymphocytes. Both B and T-cell lymphocytes have a specialised function, having an “immunological memory”. This means that when we have an infection, disease, or if some of our cells are damaged (or mutated), our lymphocytes examine these cells and create specialised “memory B or T-cells”.
These memory cells keep all the information about how to fight the infection, or repair the damaged cells if the same infection or damage happens again. This way they can destroy or repair cells much faster and more effectively next time.
- B-cell lymphocytes also make antibodies (immunoglobulins) to help fight infections.
- T-cells help regulate our immune responses so that our immune system works effectively to fight infections, but also helps to stop the immune response once the infection is gone.
Lymphocytes can become cancerous lymphoma cells
Cutaneous lymphomas happen when either the B-cells or T-cells that travel to your skin become cancerous. The cancerous lymphoma cells then divide and grow uncontrollably, or do not die when they should.
Both adults and children can get cutaneous lymphomas and most people with cutaneous lymphoma will have cancerous T-cells. Only about 5 out of every 20 people with cutaneous lymphoma will have a B-cell lymphoma.
Cutaneous lymphomas are also divided into:
- Indolent – Indolent lymphomas are slow growing and often go through stages where they are “sleeping” causing no harm to you. You may not need any treatment if you have an indolent cutaneous lymphoma, though some people will. Most indolent lymphomas do not spread to other parts of your body, though some can cover different areas of skin. Over time, some indolent lymphomas can become advanced in stage, meaning they spread to other parts of your body, but this is rare with most cutaneous lymphomas.
- Aggressive – Aggressive lymphomas are fast-growing lymphomas that can develop quickly and spread to other parts of your body. If you have an aggressive cutaneous lymphoma, you will need to start treatment soon after you are diagnosed with the disease.
Symptoms of Cutaneous Lymphoma
Indolent cutaneous lymphoma
You may not have any noticeable symptoms if you have an indolent lymphoma. Because indolent lymphomas are slow growing, they develop over many years, so a rash or lesion on your skin may go unnoticed. If you do get symptoms they may include:
- a rash that does not go away
- itchy or painful areas on your skin
- flat, reddish, scaly patches of skin
- sores that can crack and bleed and not heal as expected
- generalised redness over large areas of skin
- a single, or multiple lumps on your skin
- If you have a darker colour skin, you may have areas of skin that are lighter than others (rather than redness).
Patches, papules, plaques and tumours - What's the difference?
The lesions you have with cutaneous lymphomas can be a generalised rash, or may be referred to as patches, papules, plaques or tumours.
Patches – are usually flat areas of skin that are different to the skin around it. They can be smooth or scaly and can look like a general rash.
Papules – are small, solid raised areas of skin, and may look like a hard pimple.
Plaques – are hardened areas of skin that are often slightly raised, thicker areas of skin that are often scaly. Plaques can often be mistaken for eczema or psoriasis.
Tumours – are raised bumps, lumps or nodules that can sometimes become sores that do not heal.
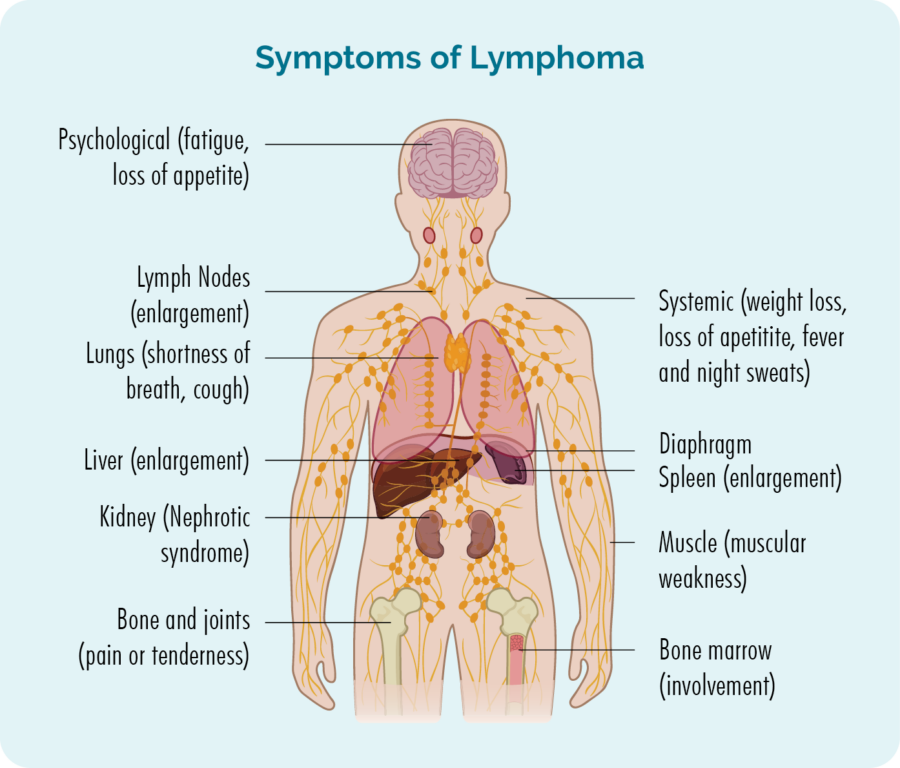
Aggressive and Advanced cutaneous lymphoma
If you have an aggressive or advanced cutaneous lymphoma, you may have any of the above symptoms, but you may also have other symptoms. These can include:
- Swollen lymph nodes that you may be able to see or feel as a lump under your skin – these will usually be in your neck, armpit or groin.
- Fatigue which is extreme tiredness not improved with rest or sleep.
- Unusual bleeding or bruising.
- Infections that keep coming back or don’t go away.
- Shortness of breath.
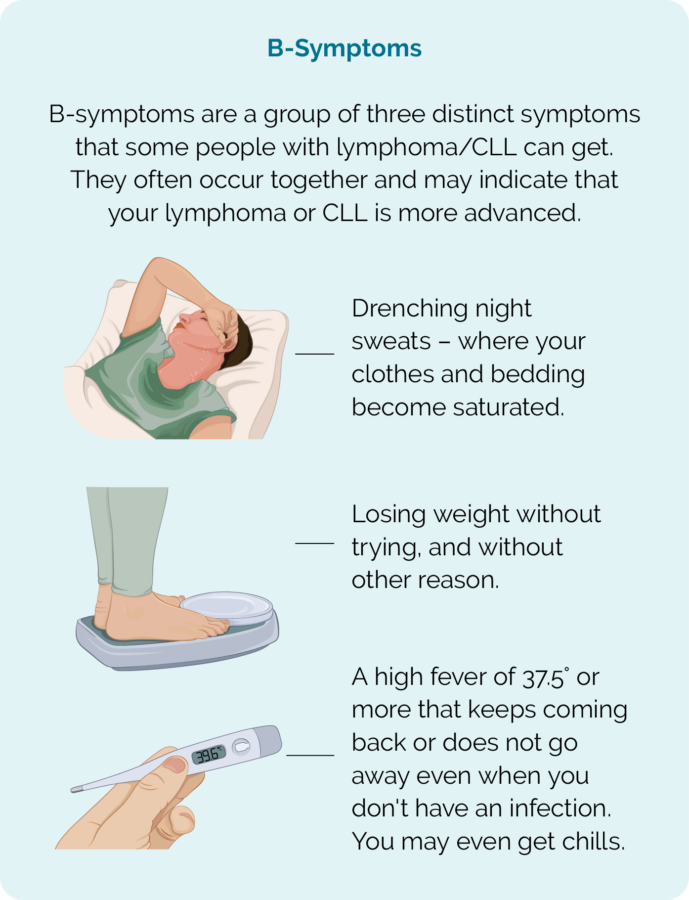
- B-symptoms.
How is cutaneous lymphoma diagnosed?
You will need a biopsy or several biopsies to diagnose cutaneous lymphoma. The type of biopsy you have will depend on the type of rash or lesions you have, where they are located on your body and how big they are. It will also depend on whether it is only your skin that is affected, or if the lymphoma has spread to other parts of your body such as your lymph nodes, organs, blood or bone marrow. Some of the types of biopsies that may be recommended for you are listed below.
Skin biopsy
A skin biopsy is when a sample of your rash or lesion is removed and sent to pathology for testing. In some cases, if you have a single lesion, the entire lesion may be removed. There are different ways to perform the skin biopsy, and your doctor will be able to talk to you about the right skin biopsy for your circumstances.
Lymph node biopsy

If you have swollen lymph nodes that can be seen or felt, or that have shown up on scans, you may have a biopsy to see if the lymphoma has spread to your lymph nodes. There are two main types of lymph node biopsies used to diagnose lymphoma.
They include:
Core needle biopsy – where a needle is used to remove a sample of your affected lymph node. You will have a local anaesthetic to numb the area so you don’t feel pain during this procedure. In some cases, the doctor or radiologist may use an ultrasound to guide the needle into the right spot for the biopsy.
Excisional biopsy – with an excisional biopsy you will likely have a general anaesthetic so you sleep through the procedure. An entire lymph node or lesion is removed during and excisional biopsy so the entire node or lesion can be checked in pathology for signs of lymphoma. You will likely have a few stitches and a dressing when you wake up. Your nurse will be able to talk to you about how to care for the wound, and when/if you need to have the stitches removed.
Subtypes of indolent cutaneous T-cell lymphomas
Mycosis Fungoides is the most common subtype of indolent cutaneous T-cell lymphoma. It usually affects older adults, and men slightly more often than women, however children can also develop MF. In children it affects boys and girls equally and is usually diagnosed around the age of 10 years.
MF usually only affects your skin, but about 1 in 10 people may have a more aggressive type of MF that can spread to your lymph nodes, blood and internal organs. If you have an aggressive MF, you will need treatment similar to the treatments given for other aggressive cutaneous T-cell lymphoma.
Primary cutaneous ALCL is an indolent (slow-growing) lymphoma that starts in the T-cells in the layers of your skin.
This type of lymphoma is sometimes called a subtype of cutaneous lymphoma and sometimes called a subtype of Anaplastic Large Cell Lymphoma (ALCL). The reason for the different classifications is because the lymphoma cells have similar features to other types of ALCL such as being very large cells that look very different from your normal T-cells. However, it usually only affects your skin and grows very slowly.
Unlike aggressive subtypes of cutaneous lymphoma and ALCL, you may not need any treatment for PcALCL. You may live with PcALCL for the rest of your life, but it is important to know, that you can live well with it, and it may not have any negative effect on your health. It usually only affects your skin and very rarely spreads past your skin to other parts of your body.
PcALCL usually starts with a rash or lumps on your skin that may be itchy or painful, but may also not cause you any discomfort. Sometimes, it may be more like a sore that doesn’t heal as you would expect it to. Any treatment of PcALCL is likely to be to improve any itching or pain, or to improve the look of the lymphoma rather than to treat the lymphoma itself. However, if the PcALCL only affects a very small area of skin, it may be removed with surgery or through radiotherapy.
PcALCL is more common in people aged between 50-60 years, but can affect anyone of any age, including children.
SPTCL can occur in both children and adults but is more common in adults, with an average age at diagnosis being 36 years of age. It is named this because it looks like another condition called panniculitis, which occurs when the fatty tissue under the skin gets inflamed, causing lumps to develop. About one in five people with SPTCL will also have an existing auto-immune disease which causes your immune system to attack your body.
SPTCL occurs when cancerous T-cells travel to and remain in the deeper layers of your skin and fatty tissue, causing lumps to come up under your skin that you can see or feel. You may even notice some plaques on your skin. Most lesions are around 2cm in size or less.
Other side-effects you may get with SPTCL include:
- blood clots or unusual bleeding
- chills
- haemophagocytic lymphohistiocytosis – a condition where you have too many activated immune cells that cause damage to your bone marrow, healthy blood cells and organs
- An enlarged liver and/or spleen.
Lymphomatoid papulosis (LyP) can affect children and adults. It is not cancer so is officially not a type of lymphoma. However, it is considered a precursor for cutaneous T-cell lymphoma such as Mycosis Fungoides or Primary Cutaneous Anaplastic Large Cell Lymphoma, and more rarely Hodgkin Lymphoma. If you have been diagnosed with this condition you may not need any treatment, but will be monitored more closely by your doctor for any signs of the LyP turning cancerous.
It is a condition affecting your skin where you may have lumps that come and go on your skin. The lesions may start off small and grow larger. They can crack and bleed before drying out and going away without any medical intervention. It can take up to 2 months for the lesions to go away. However, if they cause pain or itching or other uncomfortable symptoms you may have treatment to improve these symptoms.
If you frequently get rashes or lesions like this, see your doctor for a biopsy.
Subtypes of indolent B-cell cutaneous lymphomas
Primary Cutaneous Follicle Centre Lymphoma (pcFCL) is an indolent (slow-growing) B-cell lymphoma. It is common in the western world and affects older patients, with the average age at diagnosis being 60 years.
This is the most common subtype of Cutaneous B-Cell Lymphoma. It is usually indolent (slow growing) and develops over months, or even years. It usually appears as bumpy reddish or brownish lesions or tumours on the skin of your head, neck, chest, or abdomen. Many people will never need treatment for pcFCL but if you have uncomfortable symptoms, or are troubled by its appearance, you may be offered treatment to improve the symptoms or appearance of the lymphoma.
Primary Cutaneous Marginal Zone Lymphoma (pcMZL) is the second most common subtype of B-cell cutaneous lymphomas and affects men twice as much as women, however it can also occur in children. It is more common in older people aged over 55 years, and people who have had a previous infection with Lyme disease.
Skin changes can develop in one place, or in several places around your body. More commonly it starts on your arms, chest or back as pink, red or purple patches or lumps.
These changes happen over a long period of time, so may not be very noticeable. You may not need any treatment of pcMZL, but treatments may be offered if you are having symptoms that are causing you concern.
This is a very rare subtype of CBCL found in patients who are immune compromised and have had Epstein-Barr virus – the virus that causes glandular fever.
You will likely only have one ulcer on your skin or in your gastrointestinal tract or mouth. Most people do not need treatment for this subtype of CBCL. However, if you are taking immunosuppressive medications, your doctor may review the dose to allow your immune system to recover a little.
In rare cases, you may need treatment with a monoclonal antibody or anti-viral medication.
Subtypes of Aggressive Lymphoma
Sezary Syndrome is so named because the cancerous T-cells are called Sezary cells.
It is the most aggressive cutaneous T-cell lymphoma (CTCL) and unlike other types of CTCL, the lymphoma (Sezary) cells are found not only in the layers of your skin, but also in your blood and bone marrow. They can also spread to your lymph nodes and other organs.
Sezary Syndrome can affect anyone but is a little more common in men aged over 60 years of age.
Symptoms you may get with Sezary Syndrome include:
- B-symptoms
- severe itching
- swollen lymph nodes
- swollen liver and/or spleen
- thickening of the skin on the palms of your hands or soles of your feet
- thickening of your finger and toenails
- hair loss
- drooping of your eye lid (this is called ectropion).
Because of the fast-growing nature of the Sezary cells, you may respond well to chemotherapy which works by destroying fast-growing cells. However, relapse is common with Sezary Syndrome, meaning that even after a good response, it is likely the disease will come back and need more treatment.
This is a very rare and aggressive T-cell lymphoma that results in multiple skin lesions developing quickly on the skin over the whole body. The lesions can be papules, nodules or tumours which can ulcerate and appear as open sores. Some may look like plaques or patches and some may bleed.
Other symptoms may include:
- B-symptoms
- Loss of appetite
- fatigue
- diarrhea
- vomiting
- swollen lymph nodes
- enlarged liver or spleen.
Due to the aggressive nature, PCAETL can spread to areas inside your body including lymph nodes and other organs.
You will need treatment with chemotherapy quickly after diagnosis.
Primary Cutaneous (skin) Diffuse Large B-cell lymphoma is a rare subtype of lymphoma affecting less than 1 out of 100 people with NHL.
This is less common than other subtypes of Cutaneous B-Cell Lymphomas. It is more common in women than men and tends to be aggressive or fast growing. Which means as well as affecting your skin, it can quickly spread to other parts of your body, including your lymph nodes and other organs.
It can develop over weeks to months, and it usually affects older people around the age of 75 years. It often starts on your legs (Leg-type) as one or more lesions/tumours but can also grow on your arms and torso (chest, back and abdomen).
It is called Primary Cutaneous Diffuse Large B-cell Lymphoma because while it starts in the B-cells in the layers of your skin, the lymphoma cells are similar to those found in other subtypes of Diffuse Large B-cell Lymphoma (DLBCL). For this reason, this subtype of cutaneous B-cell Lymphoma is often treated similarly to other subtypes of DLBCL. For more information on DLBCL, click here.
Staging of Cutaneous Lymphoma
Once it has been confirmed that you have a cutaneous lymphoma, you will need to have more tests to see if the lymphoma has spread to other parts of your body.
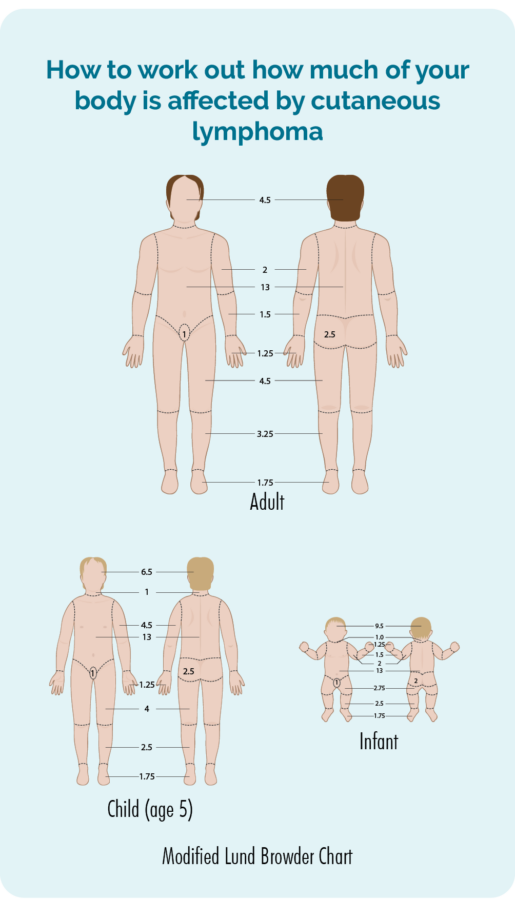
Physical examination
Your doctor will do a physical examination and check the skin all over your body to see how much of your skin is affected by the lymphoma. They may ask for your consent to take photos so they have a record of what it looked like before you start any treatment. They will then use these to check if there is improvement with the treatment. Consent is your choice, you do not have to have photos if you do not feel comfortable with this, but if you do consent, you will need to sign a consent form.
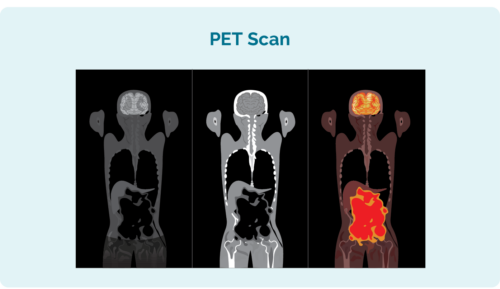 Positron Emission Tomography (PET) Scan
Positron Emission Tomography (PET) Scan
A PET scan is a scan of your entire body. It is done in a special section of the hospital called “nuclear medicine” and you will be given an injection of a radioactive medicine that any lymphoma cells absorb. When the scan is taken, the areas with lymphoma then light up on the scan to show where the lymphoma and the size and shape of it.
Computed Tomography (CT) scan
A CT scan is a specialised X-ray that takes 3 dimensional pictures of the inside of your body. It usually takes a scan of an area of your body such as your chest, abdomen or pelvis. These images can show if you have swollen lymph nodes deep inside your body, or areas that look cancerous in your organs.
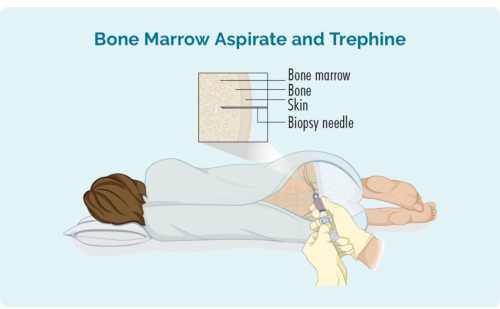
Bone Marrow Biopsy
Most people with cutaneous lymphoma will not need a bone marrow biopsy. However, if you have an aggressive subtype, you may need one to check if the lymphoma has spread to your bone marrow.
Two types of biopsies are taken during bone marrow biopsy:
- Bone marrow aspirate (BMA): this test takes a small amount of the liquid found in the bone marrow space
- Bone marrow aspirate trephine (BMAT): this test takes a small sample of the bone marrow tissue
TNM/B staging system for cutaneous lymphoma
The staging of cutaneous lymphoma uses a system called TNM. If you have MF or SS there will be an extra letter added – TNMB.
T = size of Tumour – or how much of your body is affected by the lymphoma.
N = lymph Nodes involved – checks if the lymphoma has gone to your lymph nodes, and how many lymph nodes have lymphoma in them.
M = Metastasis – checks if, and how far the lymphoma has spread inside your body.
B = Blood – (MF or SS only) checks how much lymphoma is in your blood and bone marrow.
TNM/B Staging of Cutaneous Lymphoma |
||
Cutaneous Lymphoma |
Mycosis fungoides (MF) or Sezary Syndrome (SS) only |
|
TTumouror skinaffected |
T1 – you only have one lesion.T2 – you have more than one skin lesion but the lesions are in one area, or two areas close together on your body.T3 – you have lesions across many areas of your body. |
T1 – less than 10% of your skin is affected.T2 – more than 10 % of your skin is affected.T3 – you have one or more tumours bigger than 1cm.T4 – you have erythema (redness) covering more than 80% of your body. |
NLymphNodes |
N0 – your lymph nodes appear normal.N1 – one group of lymph nodes are involved.N2 – two or more groups of lymph nodes are affected in your neck, above your clavicle, underarms, groin or knees.N3 – lymph nodes in, or near your chest, lungs and airways, major blood vessels (aortic) or hips are involved. |
N0 – Your lymph nodes appear normal.N1 – you have abnormal lymph nodes with low grade changes.N2 – You have abnormal lymph nodes with high grade changes.Nx – you have abnormal lymph nodes, but the grade is not known. |
MMetastasis(spread) |
M0 – none of your lymph nodes are affected.M1 – lymphoma has spread to your lymph nodes outside of your skin. |
M0 – none of your internal organs are involved, such as lungs, liver, kidneys, brain.M1 – lymphoma has spread to one or more of your internal organs. |
BBlood |
N/A |
B0 – less than 5% (5 out of every 100) cancerous lymphocytes in your blood.These cancerous cells in your blood are called Sezary cells.B1 – More than 5% of the lymphocytes in your blood are Sezary cells.B2 – More than 1000 Sezary cells in a very small amount (1 microliter) of your blood. |
Your doctor may use other letters such as “a” or “b” to further describe your lymphoma cells. These may refer to the size of your lymphoma, the way the cells look, and whether they have all come from one abnormal cell (clones) or more than one abnormal cell.Ask your doctor to explain your individual stage and grade, and what it means for your treatment. |
||
Treatment for Indolent Cutaneous Lymphoma
Most indolent lymphomas cannot be cured yet despite this, many people with indolent cutaneous lymphomas will never need treatment.
Indolent cutaneous lymphomas are also usually not harmful to your health, so any treatment you have will be to manage your symptoms rather than cure your disease.
Some symptoms that may benefit from treatment include:
- pain
- itching
- wounds or sores that keep bleeding
- embarrassment or anxiety related to the way the lymphoma looks.
Types of treatment can include the following.
Local or skin directed treatment.
Topical treatments are creams or gels that you rub into the area of lymphoma, while skin directed therapy may include radiotherapy or phototherapy. Below is an overview of some treatments you may be offered.
Ledaga is a newer anti-cancer topical gel that you may be offered in you have Mycosis Fungoides and it is affecting less than 25% – or a quarter of your body. The active ingredient that helps to control the MF is called chlormethine hydrochloride. It is a type of chemotherapy.
Because it is chemotherapy, you should not get pregnant, or get somebody else pregnant while using Ledaga. If an unexpected pregnancy happens, let your doctor know as soon as possible.
Always wash your hands with soap and water after applying the gel, and if somebody else puts it on for you, they must wear nitrile gloves to protect themselves. Instruct them to wash their hands after taking the gloves off.
Corticosteroids – are toxic for lymphoma cells and helps to destroy them. They can also reduce inflammation and help improve symptoms such as itching.
Retinoids – are medications very similar to vitamin A. They can help reduce inflammation, and regulate the growth of cells on the skin. They are used less commonly, but are helpful in some particular types of skin lymphoma.
Phototherapy – is a type of treatment that uses specialised lights (often UV) on areas of your skin affected by lymphoma. The UV interferes with the cells’ growing process, and by damaging the growing process, the lymphoma is destroyed.
Radiotherapy – uses X-rays to cause damage to the cell’s DNA (the genetic material of the cell) which makes it impossible for the lymphoma to repair itself. This causes the cell to die. It usually takes a few days or even weeks after radiation treatment begins for the cells to die. This effect can last for several months, meaning that cancerous lymphoma cells in the treated area/s can be destroyed even months after treatment has finished.
In some cases you may have surgery, either under a local or general anaesthetic to remove the whole area of skin affected by lymphoma. This is more likely if you have a single lesion or several smaller lesions. It is more commonly used as part of the process to diagnose your lymphoma, rather than as a cure though.
Systemic treatments
If you have many areas of your body that are affected by the lymphoma, you may benefit from a systemic treatment such as chemotherapy, immunotherapy or targeted therapy. These are described in more detail under the next section – Treatment for aggressive cutaneous lymphoma.
Treatment for Aggressive or Advanced Cutaneous Lymphoma
Aggressive and/or advanced cutaneous lymphomas are treated similarly to other types of aggressive lymphoma and can include:
Systemic treatments
Chemotherapy is a type of treatment that directly attacks fast growing cells, so it can be effective at destroying fast growing lymphomas. But it cannot tell the difference between healthy and cancerous fast-growing cells, so it can cause some unwanted side-effects such as hair loss, nausea and vomiting, or diarrhea or constipation.
Immunotherapies can help your immune system find and fight the lymphoma more effectively. They can do this in several ways. Some, such as monoclonal antibodies attach to the lymphoma to help your immune system “see” the lymphoma so it can recognise and destroy it. They are also able to affect the structure of the lymphoma cell wall, causing them to die.
- Rituximab is an example of an monoclonal antibody that may be used to treat come B-cell lymphomas including cutaneous B-cell lymphoma if they have a CD20 marker on them.
- Mogamulizumab is an example of a monoclonal antibody approved for people with Mycosis Fungides or Sezary Syndrome.
- Brentuximab vedotin is an example of “conjugated” monoclonal antibody which is approved for some other types of T-cell lymphoma that have a CD30 marker on them. It has a toxin attached (conjugated) to the antibody, and the antibody delivers the toxin straight into the lymphoma cell to destroy it from the inside.
Others, such as interleukins and interferons are special proteins that naturally occur in our bodies, but can also be taken as medicine. They work by boosting your immune system, helping it to wake up other immune cells, and by telling your body to make more immune cells to fight the lymphoma.
You may have immunotherapies on their own, or in combination with other types of treatments such as chemotherapy.
Targeted therapies are medications made that target something specific to the lymphoma cell, so they often have fewer side effects than other treatments. These medications work by interrupting the signals the lymphoma cells need to survive. When they do not get these signals, the lymphoma cells stop growing, or starve because they do not get the nutrients they need to survive.
Stem cell transplant
Stem cell transplants are only used if your lymphoma does not respond to other treatments (is refractory), or comes back after a time of remission (relapse). It is a multi-step treatment where your own, or a donor’s stem cells (very immature blood cells) are removed through a procedure called apheresis, and then given to you at a later time, after you have had high dose chemotherapy.
With cutaneous lymphoma, it is more common for you to receive stem cells from a donor rather than your own. This type of stem cell transplant is called an Allogeneic Stem Cell transplant.
Extracorporeal photopheresis (ECP)
Extracorporeal photopheresis is a treatment used predominantly for advanced MF and SS. It is a process of “washing” your blood and making your immune cells more reactive to the lymphoma to cause the lymphoma cells to be killed. If you need this treatment, your doctor will be able to provide you with more information.
Clinical Trials
It is recommended that anytime you need to start treatment you ask your doctor about clinical trials you may be eligible for. Clinical trials are important to find new medicines, or combinations of medicines to improve treatment of cutaneous lymphoma in the future.
They can also offer you a chance to try a new medicine, combination of medicines or other treatments that you would not be able to get outside of the trial. If you are interested in participating in a clinical trial, ask your doctor what clinical trials you are eligible for.
There are many treatments and new treatment combinations that are currently being tested in clinical trials around the world for patients with both newly diagnosed and relapsed cutaneous lymphomas.
Treatment options for aggressive or late-stage cutaneous lymphoma | |
B-cell cutaneous | T-cell cutaneous |
|
|
Also ask your haematologist or oncologist about any clinical trials you may be eligible for. | |
What happens when treatment doesn't work, or the lymphoma comes back
Sometimes treatment for lymphoma doesn’t work at first. When this happens it is called refractory lymphoma. In other cases, the treatment may work well, but after a time of remission the lymphoma may come back – this is called a relapse.
Whether you have a relapsed or refractory lymphoma, your doctor will want to try a different treatment that may work better for you. These next treatments are called second-line treatments, and may be more effective than the first treatment.
Talk to your doctor about what the expectations of your treatment are, and what will the plan be if any of them don’t work.
What to expect when treatment finishes
When you finish your treatment your specialist doctor will still want to see you regularly. You will have regular check-ups including blood tests and scans. How often you have these tests will depend on your individual circumstance and your haematologist will be able to tell you how often they want to see you.
It can be an exciting time or a stressful time when you finish treatment – sometimes both. There is no right or wrong way to feel. But it is important to talk about your feelings and what you need with your loved ones.
Support is available if you are having a difficult time coping with the end of treatment. Talk to your treating team – your haematologist or specialist cancer nurse as they may be able to refer you for counselling services within the hospital. Your local doctor (general practitioner – GP) can also help with this.
Lymphoma Care Nurses
You can also give one of our Lymphoma Care Nurses a call or email. Just click on the “Contact Us” button at the bottom of the screen for contact details.
Summary
- Cutaneous lymphoma is a subtype of Non-Hodgkin Lymphoma resulting from cancerous blood cells called lymphocytes, travelling to and living in the layers of your skin.
- Indolent Cutaneous Lymphomas may not need treatment as they are often not dangerous to your health, but you may have treatment to manage symptoms if they make you uncomfortable, or if the lymphoma spreads to your lymph nodes or other parts of your body.
- Aggressive Cutaneous Lymphomas need treatment soon after you are diagnosed.
- There are several different specialist doctors that may manage your care, and this will depend on your individual circumstances.
- If your lymphoma is affecting your mental health or mood you can ask your doctor for a referral to a psychologist to help you cope.
- Many treatments are aimed to improve your symptoms; however, you may also need treatments to manage the lymphoma, and these can include chemotherapy, monoclonal antibodies, targeted therapies and stem cell transplants.