Being a carer for someone with lymphoma can be both rewarding and challenging. And, although you are the carer, you will also need support to keep yourself well and rested, while managing the emotional and physical demands of being a carer.
Life doesn’t stop when you become a carer, or when someone you love is diagnosed with lymphoma. You may still have to manage work, school, children, household duties and other responsibilities. This page will provide information on what you need to know to support your person with lymphoma, and find the right supports for yourself.

Related pages
What do I need to know?
If you are going to be caring for someone with lymphoma there are some things about lymphoma and its treatments you will need to know. Below are links to other pages on this website we recommend you review as you learn about what type of care your loved one may need.
Types of carers
There are different types of carers. Some of you may be a paid carer where your sole job is to care for someone with lymphoma, but most carers are unpaid family members or friends. You may have a formal agreement about what your duties as a carer are, or you may be a friend, husband or wife, parent of a child or someone with lymphoma. In this case you may have a very informal arrangement where you provide extra support as needed within your unique relationship.
Regardless of what type of carer you are you will need extra support. The support you need will be very unique to you, and will depend on:
- your loved ones individual circumstance,
- the subtype of lymphoma they have,
- the type of treatment they will need,
- any other illness or conditions your person with lymphoma has, such as pain, symptoms of lymphoma or side-effects from treatment, difficulty with mobility and daily tasks,
- where you both live,
- your other responsibilities such as work, school, children, housework, and social groups,
- previous experience you have or haven’t had as a carer (being a carer does not come naturally for many people),
- your own physical, emotional and mental health,
- the type of relationship you have with your person with lymphoma,
- many other things that make you and your person unique.
If it is your partner, wife or husband that has lymphoma, they may no longer be able to offer you the same type of support, comfort, affection, energy or enthusiasm they have in the past. If they previously contributed to household chores, finances or raising children, they may have less capacity to do this now so more of these things may fall on you.
Your partner, wife or husband
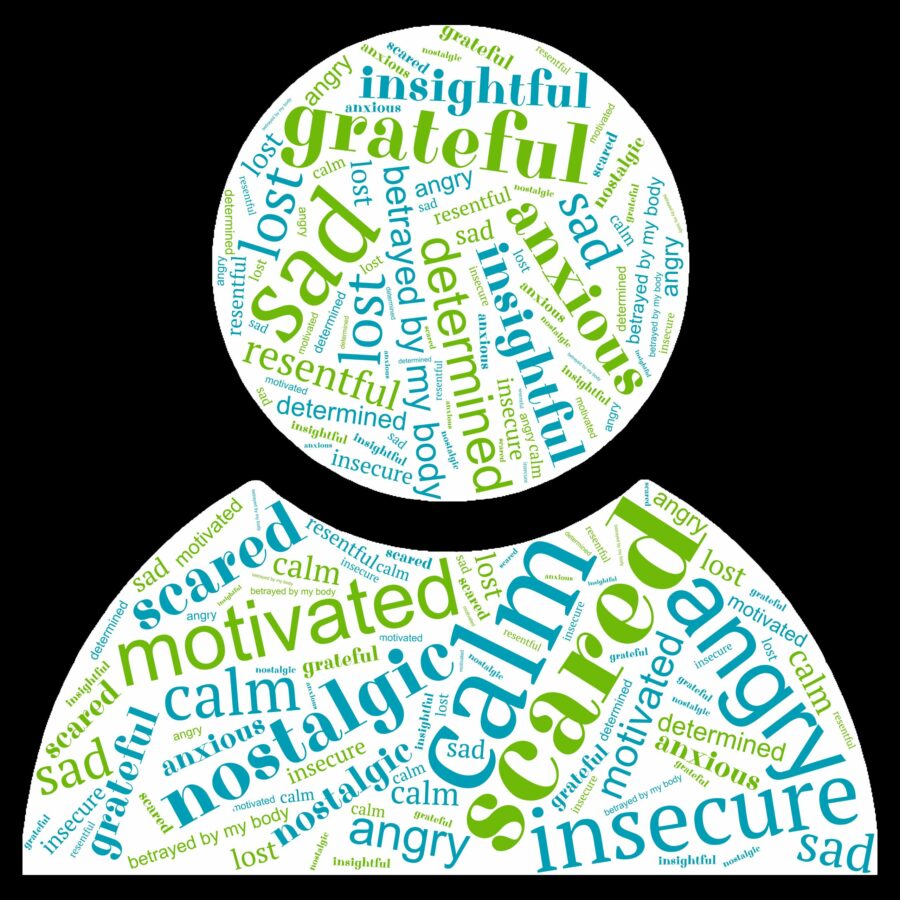
The change and imbalance in your roles will have an emotional impact on both of you. Even if they don’t express it in words, your person with lymphoma may feel a combination of positive and negative emotions as they go through lymphoma and its treatment.
They may feel:
- guilty or embarrassed that they can no longer keep up with their usual lifestyle and activities,
- afraid that your feelings for them may change,
- feel self-conscious about how the treatments change their body,
- worried about what the loss of their income may mean to your family.
With all this, they will likely still be so grateful to have you to help them through this part of their life.
They may also consider their mortality for the first time in their life, and this may cause fear and anxiety, or insightfulness as they weigh up what is really important to them and think back over their life. Even if they have a good chance of cure, it is still normal to have these thoughts and feelings.
You, the carer
Watching your partner or spouse go through lymphoma and its treatments is not going to be easy. Even if they have a good chance of cure, you may start to think about what it would be like to lose them, and this can cause fear and anxiety. You are going to have to support them through some tough times, and while this can be very rewarding, it can also be both physically and emotionally exhausting.
You will need your own support network of friends, family or health professionals as you manage all your usual activities and work while also now supporting your partner.
You may notice some role reversal in your relationship if your partner has always been the provider, or carer, or the strong and organised one. And now it is up to you to fill these roles while they concentrate on treatment and their physical health. This can take a bit of getting used to for both of you.
 Sex and intimacy
Sex and intimacy
It is very normal to wonder about sex and intimacy and how this may change when you become carer for your partner. Things may change for a while and learning new ways to be intimate will be important to maintain the closeness in your relationship.
It is still ok to have sex if you and your partner both want it, however there are extra precautions you will need to take. See the link below for more information on protecting yourself, your partner and your relationship.
Being a carer when you are still a child or young adult yourself is an enormous responsibility. You are not alone. There are about 230,000 carers in Australia just like you! Most say that it is really rewarding, and they feel good for being able to help someone they love.
That doesn’t mean it’s going to be easy. You will learn a lot, and probably make a few mistakes – But that’s ok, because we all make mistakes! And all this you may be doing while you are still at school or uni, or looking for work and trying to still have some sort of normal life too.
There is a lot of support available for you as a carer. We’ve included some links below of places that can help.
Watching your child or teenager go through lymphoma and its treatments is an unimaginable challenge for most parents. You will see your child go through things no child should have to deal with. And, if you have other children, you will have to help them learn how to cope with their brother or sister’s lymphoma and continue with their own childhood too.
Unfortunately, while still rare, lymphoma is the third most common cancer in children, and the most common cancer in adolescents and young adults in Australia. See the link below on Lymphoma in children, adolescents and young adults for more information on lymphoma in young people.
We’ve also added some links below of organisations that are dedicated to supporting children and families when someone is diagnosed with cancer. Some offer activites like excursions, camping and connecting with other kids with cancer, or who have a parent with cancer, while others may provide more practical support.
- Lymphoma in Children, adolescents and young adults
- Tips for parents & guardians
- Kids Cancer Charity & Family Support Australia | Redkite
- Camp and Retreats for Kids Facing Cancer | Camp Quality
- Canteen Connect – A Community for Young People Affected by Cancer
- Cancer Hub | Support Services for Families Facing Cancer
- Parenting through cancer
- Financial Assistance for Families – Kids with Cancer
- Sony foundation – to help with fertility preservation.
School and tutoring
If your child is school aged you may be worried about how they will keep up with school while having treatment. Or perhaps, you have been so busy with everything going on that you haven’t even had a chance to think about it.
Your other children may also miss school if your family has to travel distances and stay away from home while your child with lymphoma is in hospital.
But thinking about schooling is important. Most children with lymphoma can be cured and will need to return to school at some point. Many major children’s hospitals have a tutoring service or school that you child with lymphoma and your other children can attend while your child is having treatment or in hospital.
The below major hospitals have a school services within their service. If your child is having treatment at a different hospital than those listed here, ask them about schooling support is available for your child/ren.
QLD. – Queensland Children’s Hospital School (eq.edu.au)
VIC. – Victoria, Education Institute: Education Institute (rch.org.au)
S.A. – Hospital School of South Australia’s hospital education programs
W.A. – School in hospital (health.wa.gov.au)
N.S.W. – School in hospital | Sydney Children’s Hospitals Network (nsw.gov.au)
Whether you are a parent looking after an adult child with lymphoma, or an adult looking after you parent with lymphoma, or a friend caring for a friend, there will be changes to the dynamics of your relationship.
Parent carers
As a parent caring for your adult son or daughter you may need to make many changes to your lifestyle. This can be tricky if you have other commitments. The dynamics of your relationship may also change as your adult child once again becomes dependent on your care and support. For some this can bring you closer, for others it may be challenging. Your GP can be a great support. Some services they may be able to refer you to are listed further down the page.
Confidentiality
Your adult child has the right to confidentiality of their health records. They also have the right to choose to go appointments alone, or with who they choose.
It can be very difficult as a parent to accept this, but some people do cope better when they don’t have to share everything. It is important to accept their decision on how much information they want to share with you. However, if they do want you to go with them, it is a great way to show support and keep up to date with what they may need.
Ask them what they would prefer and respect their decision.
Caring for a parent with lymphoma
 Caring for a parent with lymphoma can be very rewarding and a way of showing your love and appreciation for everything they have done for you. However, it can also come with challenges.
Caring for a parent with lymphoma can be very rewarding and a way of showing your love and appreciation for everything they have done for you. However, it can also come with challenges.
A parent’s role is to protect their children, so sometimes it can be a hard for a parent to become reliant on their kids – even grown-up kids. They may want to shield you from the reality of what they are going through or feeling, and may not share all the information you feel you need to support them.
Many older people don’t want too much information and would prefer to leave decision making up to their specialist doctor. This can be difficult when you’re a parents’ carer.
It is important to respect your parents right to confidentiality and also their independence.
Having said that, you still need enough information to be able to care for and advocate for your parent. Getting the balance right can be tricky and take time and practice. If your parent agrees, try to go to as many of their appointments with them. This will give you an opportunity to ask questions and have a better idea of what is happening. Know that your parent does not have to agree to this, but if they do, it is a great way to build a rapport with the healthcare team and keep up to date.
Extra support is available through your GP.
Caring for a friend
Caring for a friend with lymphoma will change the dynamics of your friendship. What brought you together as friends and the things you used to do together will change. This can be challenging, but many people find their friendship becomes much deeper than it was before lymphoma.
You will need to care for yourself too and know that your friend will not be able to offer the same support and companionship as they did before. At least not for a while. We have some great tips further down the page on how to support your friend and maintain your friendship while also being their carer.
Balancing caring with work, children and other responsibilities
A diagnosis of lymphoma often comes without any warning. And sadly, very few potential carers are independently wealthy. You may be working, studying or looking for work. And we all have bills to pay. You may have your own house to keep in order, possibly children of your own and other responsibilities.
None of these responsibilities change when an unexpected lymphoma diagnosis happens to your loved one, or when their health changes and they need more support from you than before. You need to take time to realistically plan how much time you have to care for your loved one.
You may need to get a group of people, brothers and sisters, friends or others who can share the load. Even if they do not take on an official carer role, they can certainly help with some of the practical aspects of caring such as help with housework, picking up kids, cooking meals or doing shopping.
Further down the page under the section Tips for carers are some dot points that link to different websites or apps that can help coordinate the support you may need.
Emotional impact of lymphoma
Lymphoma has an emotional impact on everyone affected by it. But it often seems to affect the patient and their loved ones differently, and sometimes at different times.
No matter how hard you try, you will never fully understand what it is like for your person with lymphoma. Likewise, no matter how hard they try, they will never really understand what it is like for you watching them go through lymphoma, it’s treatments and adjusting to being forced into a life of scans, tests, treatments and feeling unwell or insecure.
Depending on your relationship with your person with lymphoma, the impact it has on your relationship will come with different challenges.
Being diagnosed with cancer is not a normal thing. Sadly, it is increasingly common, but certainly not normal. So there is no normal way to respond to the news of cancer or the challenges it brings.
Every person's experience will be different. Even within families, every family member will have different thoughts, feelings and reactions to the news of themselves or a loved one having cancer.
Treatment is often hardest on the carer – Finishing treatment is often harder on the person with lymphoma!
A diagnosis of lymphoma is hard on everybody! Life is going to change for a while, and possibly forever to some degree. While not everyone with lymphoma needs treatment straight away, many people do. But even when treatment is not needed straight away, there are still emotions around the diagnosis, and still extra tests and appointment needed that can cause anxiety and stress.
If your person is not starting treatment straight away, you may find the below webpage helpful.
In the lead up to a formal diagnosis and then staging tests and starting treatment, life will be busy. As a carer, you may need to take the lead on many of these things, making appointments, driving to appointments and being with your person during some of the most difficult news they’ll hear and decisions they have to make.
During this time, your person with lymphoma may go into business mode. Or may be in denial, or just too sick to really deal with the emotions of what is happening. Or perhaps they will have a good cry and need you by their side to comfort and support them as they come to terms with how they feel. They may leave everything to you while they concentrate on getting through treatment.
Tips for carers in lead up to, and during treatment
- Have a book, diary or folder on your device to keep track of all appointments.
- Fill out the Connect with us form to make sure you and your person with lymphoma has access to updated information on their lymphoma subtype, treatments, events and a treatment support kit when treatment starts. You can fill in the form by clicking here.
- Take some healthy snacks and drinks to appointments – sometimes delays can happen and treatment days may be long.
- Ask your person how much information they would like to share with others. Some people like to share everything while others like to keep things private. Think about how to share information, some ideas may include:
- Start a private Facebook (or other social media) page that you can share with the people you want to keep updated.
- Start a group chat on a messaging service such as WhatsApp, Facebook Messenger or similar to send quick updates to.
- Start an online Blog (diary) or VLOG (video diary) to share.
- Take notes during appointments to refer back to later, or alternatively ask the doctor if you can record the appointment on your phone or other recording device.
- Write down in your book, diary or phone your person’s subtype of lymphoma, allergies, symptoms, name of treatments and side-effects.
- Print off or download Questions to ask your doctor to take to your appointments – and add any extra you or your person may have.
- Have a bag packed for any unexpected hospital stays to keep in the car or by the door. Pack:
- toiletries
- pyjamas
- comfortable loose-fitting clothes
- non-slip well-fitting shoes
- phone, laptop, tablet and chargers
- toys, books, puzzles or other activities
- snacks.
- Delegate – call on you family and social groups to see who may be able to help with some practical things such as shopping, cooking meals, visiting, cleaning the house, picking up kids from school. Some of the following apps may be useful:
Does your person with lymphoma have children?
- Kids Cancer Charity & Family Support Australia | Redkite
- Camp and Retreats for Kids Facing Cancer | Camp Quality
- Canteen Connect – A Community for Young People Affected by Cancer
- Cancer Hub | Support Services for Families Facing Cancer
And then treatment starts!
 We often hear from patients that treatment was easy compared with life after treatment. That doesn’t mean treatment is easy. They will still be fatigued and have side-effects from treatment. But many people are so overwhelmed and busy with getting through treatment that they may not have time to process what is happening – Until treatment ends.
We often hear from patients that treatment was easy compared with life after treatment. That doesn’t mean treatment is easy. They will still be fatigued and have side-effects from treatment. But many people are so overwhelmed and busy with getting through treatment that they may not have time to process what is happening – Until treatment ends.
As the carer, if life wasn’t busy enough before, it certainly will be once treatment starts! There are different types of treatment for different people and different subtypes of lymphoma. But most treatments last for months (4-6 months) at a minimum, and some can last for years.
Ongoing appointments
As well as treatment, your person will also need regular blood tests, appointments with their haematologist or oncologist AND local doctor (GP) and possibly regular PET/CT or other scans too. They may even need other tests to monitor how their heart, lungs and kidneys are coping with treatment.
Side-effects
Every treatment has potential side-effects, the type of side-effect may be different depending on the type of treatment. Different people having the same treatment can also have different side-effects or the severity of side-effect may be different.
As a carer, you will need to know about these side-effects so you can support you person at home, and know when to contact the doctor or attend the emergency department. Make sure you ask about the side-effects for the particular type of treatment your person is getting. Their haematologist or oncologist, specialist nurse or pharmacist will be able to help you with this. You can also ring our nurses on 1800 953 081 to find out more if you need to.
Once you know what side-effects your person may get, visit our side-effects page by clicking the link below to learn more about them.
Medicine may affect their mood and emotions
Some treatments for lymphoma, as well as other medicines they may be taking, along with the stress of lymphoma can affect your persons mood and emotions. This can make them teary, angry or short tempered, frustrated or sadder than normal. Learn more about this at our webpage Mental health and emotions.
It’s important to remember that these changes in mood and emotions is not about you or how well you are doing as a carer. Nor is it a true reflection of their real feelings. It is a reaction to how the medication affects different hormones and signals in the brain.
If you are concerned with how the changes in their mood and emotions is affecting them, you and others, encourage them to talk to their doctor about it. If you go to appointments with your person, you can also talk to the doctor about these changes. In many cases, this can be improved with a change in medication or dose.
Confidentiality
As difficult as this may be, as a carer you are not entitled to all your persons medical records or information. Hospitals, doctors, nurses and other health professionals are bound by confidentiality laws and cannot share medical information or records with you without very specific, and often written consent from your person.
Your person also has the right to only share what they are comfortable sharing with you. You need to respect this even if you are married, in a committed relationship or the parent or child of the person with lymphoma. Some people need time to process the new information and make a plan in their own head before they are comfortable sharing the information. Others may want to protect you from the stressors they are under.
How much or little they share with you is no indication of their love for you or how much they trust you. It is simply an individual coping mechanism for many people.
If you would like more information, let your person with lymphoma know that when they are ready, you would like to know more so you can support them as best as possible, and make any plans you may need to make. But also let them know you respect their right to privacy.
Your person may find finishing treatment harder than treatment itself!
We often hear from people with lymphoma that they were ok while going through treatment, but the months after finishing treatment was a real challenge. Finding where they fit back into life, family, work/school or social groups can take time. Many people have told us they felt lost during the months after treatment ends.
Many people with lymphoma will also have ongoing fatigue, and other symptoms or side-effects of treatment that can last for months after treatment. Some may even have long term side-effects that need ongoing management for life. So the lymphoma experience does not end when treatment does.
For some people, the emotional impact of having been diagnosed with lymphoma and having treatments doesn’t hit until after the busy-ness of appointments, scans, tests and treatments ends.
Reasonable expectations
One of the things we hear a lot from patients is that everyone expects them to get back to normal now treatment has finished. This is an unrealistic expectation!
On the other hand, some people are frustrated by their loved ones not letting them get back to some level of normality.
Ask them what they need!
The only way to know what your person needs is to ask them. Understand that it may take some time for them to regain confidence, and they may never get back to exactly where they were before. But this doesn’t have to be a bad thing. It is a great time to remove unnecessary stressors from your life and concentrate on the important things.
Making plans
Some people find it helps to make plans to look forward to something when treatment ends. However, some people may not feel confident to plan anything until after they have had some time to recover and had repeat scans to be sure the lymphoma is cured or in remission. Whatever works for your person is ok. There is no right way to handle this.
However, you may feel that you need to make plans even if your person isn’t yet ready. This is very reasonable, and the important thing is to keep communicating with each other to find a plan that works for both you.
Support available
No carer should ever have to care alone. It is important for you to connect with different people – both personal friends and family and health professionals.
Let people know what you need
Believe it or not, most people want to help. The problem is, many people don’t know how. Most people get no training or experience about how to talk about, or handle difficult things like illness.
Many people are worried that if they try to talk to you about your situation, they may upset, offend or embarrass you. Others just don’t know what to say. So many people decide to only talk about it if you bring it up. This does not mean they don’t care.
But you seem fine!
If you only catch up with friends and family when you are energetic, looking your best and telling them everything is fine, then how can you expect them to know you need help?
Let people know what you need. Let people know you are open to chatting and sharing your troubles. This can take practice. And you may not always get the response you were hoping for, but you can’t expect people to know what you need unless you let them know.
Don’t expect them to guess! It would be great if people could read our minds, but they can’t and its unrealistic to expect people to know what you need, because everybody’s situation and needs are different.
Think about some of the below networks that you may be able to talk to or ask for support from.
You may be able to lean on the leaders of your faith and congregation for emotional, spiritual and practical help. Make a time to speak with them and let them know what you are going through and ask what support hey may be able to offer.
If you are comfortable with the idea, ask them if they can put something in their newsletter or other regular communication with other members to ask for practical help whether it be regular or as a once off. You may even be able to do this anonymously with only those who approach the leader of the congregation given your details.
Many people belong to sporting or other social groups. If you have a group and have connected well with some members, talk to them about how your life is changing due to your new role as a carer. Let them know what you need help with and ask if they know of anyone who could help.
If you are comfortable with the idea, ask them if they can put something in their newsletter or other regular communication with other members to ask for practical help whether it be regular or as a once off. You may even be able to do this anonymously with only those who approach the leader of the group given your details.
Even though you’re not the one with lymphoma, it is still important for you to be connected with a GP. GPs can be a great form of support and help you coordinate the care you may need.
We recommend everyone with lymphoma and their carers have mental health plan done with your GP. This can look at the extra stressors and responsibilities you now have and make a plan to make sure you are support with counselling, psychologist, medicine or other support you may need.
You may even have medical conditions yourself that you need to manage while caring for your person. Your GP can also do a GP management plan to make sure these things don’t get missed while you are busy caring for your loved one. They can also help connect you with local organisations that can help you.
Extra Services your GP can refer you to
It is important to get the help you need to manage with these changes. Talk to your GP about support services available in your area. They can help coordinate care for you by referring you to different services in the community. Some that may help include the following.
- Psychologists or counsellors to help with the emotional and mental challenges that come with supporting someone with lymphoma.
- Occupational therapists who can help assess your needs and help get the right physical support to care for your person.
- Social workers who can help you access different social and financial supports.
Most hospitals have a social work department. You can ask to be referred to the social worker at your hospital. If your hospital doesn’t have a social work department, your local GP can help connect you with one in your community.
Social workers can help with counselling, referrals to different services for extra support, coordinating your loved one’s care, and advocating on your behalf.
They can also help you access financial support, travel assistance and accommodation or other health and legal services if needed.
Carer Gateway is an Australia Government program offering free emotional and practical support to carers’. You can find more information about them here: Carer Gateway.
Our Lymphoma Australia nurses are available Monday – Friday 9am to 4:30pm.
You can contact them by phone on 1800 953 081 or email nurse@lymphoma.org.au.
They can answer your questions, listen to your concerns and help you find support services for your loved one or yourself.
Lymphoma Down Under is an online peer support group on Facebook. It is moderated by Lymphoma Australia but is for patients and their loved ones. Many people find chatting with others with lymphoma or caring for those with lymphoma and hearing their stories really helpful.
You can join by answering the membership questions and agreeing to group rules here: Lymphoma Down Under.
Financial help for carers
You may be able to get an allowance from Centrelink to help as you care for your loved one. Both yourself, and the person you are caring for will need to meet certain requirements for you to be eligible.
Information on carer’s payments and carers allowance can be found on Services Australia webpage.
Maintaining friendships and other relationships
Many people notice changes in their friendships and family dynamics when living with cancer. Some people find that those closest to them become more distant, while others they have not been close with, come closer.
Unfortunately, many people haven’t been taught how to talk about illness and other difficult things. When people back away, it is often because they don’t know what to say, or are scared anything they do say, will upset you or make things worse.
Some may worry about sharing their own good or bad news, or feelings with you. They may not want to burden you while you are unwell. Or, they may even feel guilty when things go well for them when you have so much going on.
Tips on how to maintain relationships with friends and family
You can help your friends and family understand that is ok to talk about lymphoma or treatments your loved one is having if they want. Or even talk about what is happening in their life. If you are comfortable talking about you situation, ask questions like:
- What would you like to know about lymphoma?
- What questions do you have about (your loved one’s) treatment and side-effects?
- How much do you want to know?
- Things are going to be different for me for a while, how can we stay in touch?
- I’m going to be really busy supporting my loved one for a while. I may need some help with things like cooking, cleaning, taking care of the kids. What can you help with?
- I still want to know what is happening with you – Tell me the good the bad and the ugly – And everything in between!
- I don’t want to talk about lymphoma but ask me about (whatever you would like to talk about).
- Know any good jokes? I need a laugh.
- Can you just sit here with me while I cry, or think or rest?
- If you have the energy, you could ask them – What do you need from me?
Let people know if it is ok to visit, or how you would prefer to stay in touch
Treatments can lower your loved ones immune system. It is important to let people know that it may not always be safe to visit, but that when they do they can still hug you.
- Let them know to stay away if they are sick. Consider other ways stay in touch.
- If you are comfortable hugging people and they are well, let them know you need a hug.
- Watch a movie together – but in your own homes on a zoom, video or phone call.
- Open up a group chat on one of the many messaging or video services available.
- Start a roster, for when visiting is welcome and what you need done. The apps above can help with this.
And finally, if you notice the relationship is changing, talk about it. Let people know they still matter, and you still want to maintain the closeness you had before.
Other Resources
Summary
- The role of carer is a very individual one based on your relationship with your person with lymphoma and their individual needs.
- Carers may be family members, friends or from a paid service.
- Anyone can be carer including children and you may have a formal or informal caring role.
- As a carer you are not alone, there are services available to support you, and some payments you may be eligible for.
- Understanding lymphoma, its treatments, and side-effects will help you understand how to support your person better.
- Your person may still need your support as a carer long after treatment finishes.
- Even though you are the carer, you will need support too. Let people know what you need.
- Find a good GP and keep in regular contact with them. They can help coordinate different support services you may need.
- You can call one of our nurses on 1800 953 081 Monday – Friday 9am-4:30 pm Brisbane time.