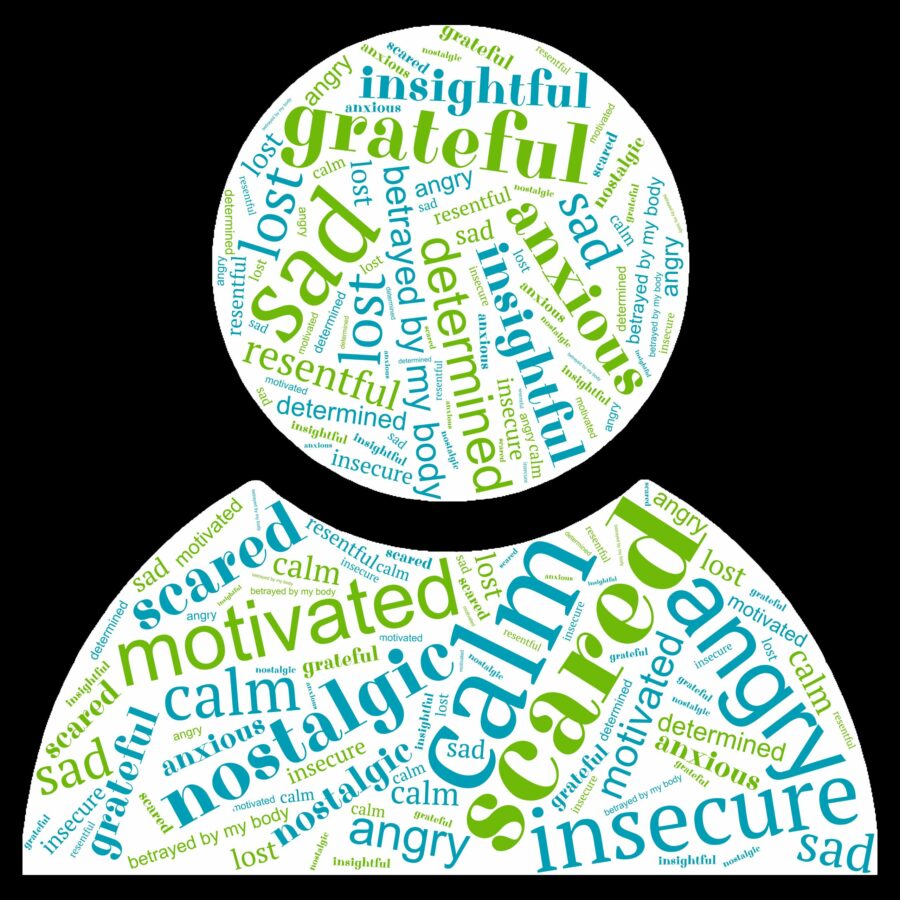
Being diagnosed with lymphoma and its treatments can have an impact on your mental health and emotions. There are many feelings you may experience, and some might even surprise you. In fact, you don’t even have to be the one diagnosed with lymphoma to be affected by changes to your mental health and emotions. Many family members and loved ones can also be affected.
This page provides information on what can cause changes in your mental health and emotions and provides some practical tips on how to manage them. We have links to some really useful videos with great information from the experts at managing different aspects of your care.
Make sure you bookmark or save this page as you may want to come back often or read it in stages.
What causes mental health and emotional changes
The shock of diagnosis, changes in your role in your family, workplace or social groups, fear of the unknown, loss of your sense of safety and security in your own body, unwanted changes to your lifestyle and fatigue or other symptoms of lymphoma can all affect your mental health and emotions.
Some medicines are known to have an impact on emotional regulation and mood. These can include corticosteroids, such as dexamethasone or prednisolone that are often given along with chemotherapy. Emotional effects from these medications can start soon after taking them, and last for several days after you stop taking them.
It is thought this side-effect is caused by the corticosteroid interfering with a naturally occurring chemical called serotonin. Serotonin is produced in our brains and is considered a “feel good” chemical that helps us to feel happy or content.
You may only notice small changes in your emotions or “patience”. However, if your mood changes a lot, or you become very sad, have feelings of hopelessness, get angrier much easier than usual or find the effects unbearable, TALK TO YOUR DOCTOR.
Your haematologist or oncologist who prescribed the corticosteroid for you need to know about these changes. There are other options, and they may just need to swap the medication to a different one to improve your symptoms, while still making sure you get the best outcomes for your treatment.
Many other medicines you may take can also impact your mood. Although they may not be part of your treatment protocol, you may be on them to manage other conditions or side-effects of treatments. If you are taking any of the below medicines and have concerns about your mental health or emotions, talk to your doctor about it.
Proton pump inhibitors
These are given to protect your tummy or if you get a lot of heartburn or indigestion. They help by reducing the acid in your stomach. Common proton pump inhibitors are pantoprazole (Somac), omeprazole (Losec) and esomeprazole (Nexium).
Anticonvulsants
These medications can also be used to help with nerve related pain and peripheral neuropathy. Common anticonvulsants used for these conditions include gabapentin (Neurontin) and pregabalin (Lyrica).
Statins
Statins are medicines given to lower the cholesterol in your blood. Common statins include atorvastatin (Lipitor), rosuvastatin (Crestor).
Benzodiazepines
These medications are often prescribed to help with short-term anxiety or short-term insomnia. They can be addictive and also have effects on your mood. Common benzodiazepines include diazepam (Valium) temazapam (Temaze or Restoril) and alprazolam (Xanax).
Polypharmacy
Polypharmacy is a term used when you are taking several different medicines, which is common during and after treatment for lymphoma, and in older people. The more medicines you take, the higher the chance of them having an interaction with each other, increasing or decreasing the effects of each medicine. If you are taking more than 5 different medicines ask your doctor to review them. You can also ask you pharmacist for advice on polypharmacy.
In some cases, there may be 1 medicine that can work in different ways that could replace 2 different types of medicines.
Pain makes everything else in life harder to deal with, and the pain itself can be distressing. Long-term or severe pain is a common cause of a depressed mood and changes in mood.
If you have pain it is important to know the cause and get the right treatment or support needed to manage it. There are different types of pain, and the pain killers (medicine) you have used in the past may not work for the type of pain you have now.
Report all severe or ongoing pain to your doctor so they can assess you to see what is causing your pain and give you the right information to improve it.
Fatigue can impact every area of your life, and your mental health and emotions can suffer when you are fatigued or unable to get a night’s sleep. Further down the page we have a video with some tips on managing fatigue, and improving your quality of sleep.
Unfortunately, some people may experience traumatic medical events. These may relate to severe reactions to medicines, life-threatening infections, multiple attempts to get a cannula in, or the diagnosis of lymphoma itself may be traumatic for some people. You may even have befriended people in hospital who may have lost their life to lymphoma or another cancer.
All these things can impact your mental health and can make it even harder to go to your appointments for checkups or treatment. In rare cases, some people have even been diagnosed with Post Traumatic Stress Disorder because of their experiences with their cancer diagnosis and treatments.
If you are struggling with the memories of past experiences in hospital, or related to your lymphoma, it is very important that you speak to your doctor about it. There are treatments available than can lessen the impact these memories have on your quality of life, and help you to remember them without the intense emotional fear that can sometimes be associated with traumatic memories.
A diagnosis of lymphoma and its treatments is likely to have a profound effect on different relationships you have. Your role in your family, social groups, school, or at work may change and these changes can have an impact on your mental health.
At home
Whether you have always been the provider of finances or emotional support, the one that keeps the house tidy and clean, the carer, the person that runs people around to different social engagements or the “life of the party” you may notice changes.
You may no longer have the energy to keep up your usual routine, or you may be experiencing symptoms or side-effects that affect your ability to maintain that routine. This means other people in your life may also need to change their role in order to support you more while you concentrate on treatment and healing.
Some of you may find this difficult, and you may experience different feelings such as sadness, guilt, anger, fear or embarrassment. Try to remember that everyone needs help sometimes, and your lymphoma diagnosis is NOT YOUR FAULT. You did not do anything to bring this illness on yourself. Lymphoma is not a cancer that is caused by your life choices.
Are you the parent of a child with lymphoma?
Watching your child go through any illness is distressing for a parent, but when it is cancer with potentially life-threatening, or life altering consequences, it can be even more difficult. As a parent, your job is to protect your children and now everything may feel out of your control. You have to rely on medical professionals to protect your child and recommend what’s best for your child. You may not understand what they are talking about half the time and have to just rely on them to make the best choices for your child.
You may watch your child lose their innocent carefree childlikeness to taking on a more mature approach to life. Or you may watch them suffer with pain, nausea, fatigue and other symptoms of lymphoma and side-effects of treatment.
For more information on childhood and adolescent lymphoma and more support services available please click here.
Work or Study
It’s up to you how much information you give your teachers, boss, Human Resources (HR) department and workmates about your lymphoma and treatments. You have a right to confidentiality that must be respected.
However, if you need to start treatment or you become unwell, you may need time off school or work, or you may need changes to your usual workspace or routine. To understand what changes, you may need to your work life, your boss or HR department will need some information, including a medical certificate outlining what you can and cannot do.
To learn more about how to manage work or study and lymphoma click here.
Social groups
Your social groups may include sporting, church, community or friendship groups, all of which may be affected by your lymphoma. Or your role or ability to participate in these groups may change for a while. However, these groups can also be a great source of support for you too if you let them know what you need.
Many people choose not to share what they are going through, but when you let people know what you need, they are better able to support you in the way you need them to.
To learn more about how to maintain romantic and other relationships when you have lymphoma click here.
Finding you out have cancer can be scary, and for some people even traumatic. Not knowing how the lymphoma will affect your life, whether it is curable or not, or living with the fear of a relapse can be a burden that affects your ability to enjoy life the way you use to.
It is normal to have some fear. But, getting the right information and asking the right questions can help you sort through the fear of the unknown and give you direction on how to move forward.
If fear is stopping you from enjoying life, or is becoming your main focus of thought, talk to your doctor or nurse so they can help you get the support you need to work through and manage the fear.
You may find that the expectation of others does not match your own expectations, or abilities. For some people, the people around you may want to protect you from anything and everything and leave you feeling like you need room to breathe, and learn your new limits.
While others may look at you and think you look well, so you must be well. Then expect you to carry on like everything is normal.
It is really hard for people to know what you need, and as much as we wish they could sometimes, they will never truly understand how you feel and what you are going through…..unless you communicate openly and honestly with them.
Let people know what you need!
Tell them if you feel they are protecting you too much or expecting too much from you.
Let them know if you are having symptoms or side-effects that are affecting you. Don’t always say you are doing ok when you are asked how you are. If you say you are ok, how can you expect them to know you are not?
Ask for help when you need it.
Share the symptoms of lymphoma and side-effect pages with your loved so they know what to expect to.
When lymphoma is in your brain, or there is a high chance it will spread there you may have treatments that may cause some changes in your mood and how you regulate your emotions. The lymphoma itself, if it is in your brain can also impact your mental health and emotions.
Report all changes in your mental health and emotions to your haematologist, oncologist or radiation oncologist so they can assess if your lymphoma or treatments may be the cause.
Finishing treatment is a time of many emotions, you may feel relieved, triumphant, scared and uncertain of what happens next.
See our finishing treatment page for information on what to expect and support available once treatment ends.
Signs & Symptoms
Changes to your mood and emotions may be subtle and hard to recognise, or very obvious. Some symptoms may even overlap with possible symptoms of lymphoma and side-effects of treatments, which can make it difficult to know how to manage. It’s important to be aware of the changes in your mood and emotions so you can get extra support when you need it.
Report any of the below signs and symptoms to your doctor.
- Loss of interest in things you used to enjoy.
- Deep feelings of sadness.
- Feeling hopeless and unable to be helped.
- Feeling of dread.
- Repeatedly replaying traumatic events in your head or having flashbacks.
- Extreme worry (anxiety).
- Fatigue.
- Difficulty sleeping or nightmares or night terrors.
- Sleeping too much and difficulty getting up.
- Total loss of energy and motivation.
- Problems with thinking, problem solving, memory or concentration.
- Changes to your weight, loss of appetite or overeating.
- Feeling irritable and restless.
- Having feelings of guilt.
- Thoughts of harming yourself or others, or of suicide.
How can I help myself feel better?
The first step to helping yourself feel better is knowing what’s causing the changes in your mental health, and you may have more than one cause. In some cases, you may need to reach out to counsellor or psychologist to help you accept and learn new coping strategies to live with the changes in your life.
In other cases, you may just need to understand that the medicines you need will make you more emotional for a few days each cycle of chemo, but understand that things will get back to normal in the days after you stop taking them.
What does the research say?
A lot of research has gone into mental health and there are many non-medical things you can do to help improve your mental health. Below are some things that research has proven to be helpful in managing your mental health and emotions
A good sleep routine
Getting the right amount of quality sleep each night has a very big impact on mental health and emotional regulation. When we’re tired, everything seems harder to cope with – whether we have lymphoma or not!
However, getting a good night sleep is easier said than done right?
Watch the video for tips on improving sleep.
Exercise
Many studies have shown that exercise has a really good effect on mood and emotions. It may be the very last thing you want to think about if you are tired and feeling down. But, getting some gentle exercise and a little sunlight every day can really help improve fatigue levels and your mood.
Even a 10-minute walk in the sunlight each morning can help set you up for a better day. Watch this video to learn from an exercise physiologist how to so some exercises even when you have no energy.
Nutrition
Eating well is important when you have lymphoma and when you are having treatment. Getting the right number of calories and a well-balanced diet is needed to improve energy, keep you blood sugar levels steady and to replace damaged cells and repair wounds. Improving all these can also improve your mental health.
But there are so many myths around about what you should and should net eat when you have cancer. Watch this video to learn from a university qualified dietician about diet, nutrition and lymphoma.
Find a psychologist near you
Speaking with a psychologist and help with all cancer related issues from first diagnosis, right through to finishing treatment, reintegrating back into life and beyond. They can help with coping strategies, building resilience and making a plan for when stress and anxiety are likely to impact your quality of life.
To find a psychologist near you click the link below.
Listen to feel good music
Music has can have a huge impact on our emotions and mood. Sad music can make us feel sad, happy music can make us feel happy, motivational music can give us energy and confidence.
We asked some of our lymphoma patients about their favourite feel-good songs and made a playlist out of these. Checkout the playlist at our Spotify channel here.
When should I see my doctor?
Changes in your mental health and emotions can range from mild to life-threatening. Your local doctor (GP) can be a great support. We recommend everyone with lymphoma, and your loved ones see their GP and ask them to do a mental health plan together. You can do this even before you notice any changes to prepare for the challenges that you may face in the future.
To learn more about getting a mental health plan done with your GP, click here.
Thoughts of hurting myself, or of suicide
Ring 000 if you have thoughts of hurting yourself or of suicide. There is help available to keep you safe! You can also find more information on support to keep you safe when you are having thoughts of suicide by clicking the button below.
Take Charge!
Watch the video below for tips on how to build resilience to improve your mental health during times of uncertainty.
Lymphoma Care Nurses
Our nurses are all qualified and highly experienced nurses who have worked with people with cancer for many years. They are here to support you, encourage you and provide you with information abut your disease, treatments and options. They can also help you find the right support to improve your mental health. Contact them by clicking on the Contact Us button at the bottom of the screen or clicking here.
Other useful resources and contacts
Summary
- Changes in your mental health and emotional regulation are common when you or your loved on has lymphoma.
- Mental health changes can happen as a result of the stress and anxiety of lymphoma, as side-effect of treatment, traumatic healthcare experiences, or a response to how lymphoma changes your life.
- Corticosteroids are a very common cause of mood and emotional changes. They usually only last while you are on the medicine and for a few days after. If these changes are affecting your quality of life, talk to your haematologist or oncologist.
- A good diet, sleep pattern and regular exercise, as well as some exposure to sunlight can help improve mental health and regulation of emotions.
- See your GP as soon as possible and do a mental health plan with them.
- Report all signs and symptoms of changes in your mental health to your haematologist or oncologist and GP.
- Reach and get help. If you have thoughts or hurting yourself, or of suicide call 000 immediately or see https://www.lifeline.org.au/get-help/i-m-feeling-suicidal/