Overview of ATLL
Adult T-cell Leukemia-Lymphoma is a very rare subtype of T-cell Non-Hodgkin Lymphoma (NHL). It can affect adults of any age but is more common in people aged 60 years or more. While being a subtype of NHL, it can be further grouped as a subtype of Peripheral T-cell Lymphoma (PTCL).
Knowing ATLL comes under both the headings of NHL and PTCL can be handy if you are looking for clinical trials you might be able to join, as not all trials will list individual subtypes of lymphoma. You may be able to join clinical trials that are looking for people with:
- Non-Hodgkin Lymphoma
- Peripheral T-cell Lymphoma
- T-cell Lymphoma
- Adult T-cell Leukemia Lymphoma.
ATLL happens when changes occur in the genes inside your T-cells, that tell the T-cell lymphocyte how to grow and work. As a result of these changes, the T-cells develop into cancerous cells and can no longer work properly. It is often aggressive, which means it grows and spreads through your body quickly.
However, there are 4 different subtypes of ATLL, and 2 of them may be indolent, which means they grow slowly and can often go through periods where they don’t grow at all, almost like they are sleeping. Indolent ATLL are very rare, and in some cases can transform into one of the more aggressive ATLL’s over time.
Aggressive ATLL needs to be treated very quickly after you are diagnosed, but if you have an indolent lymphoma you may not need treatment at all for months or even years. In very rare cases, you may never need treatment.
About T-cell Lymphocytes
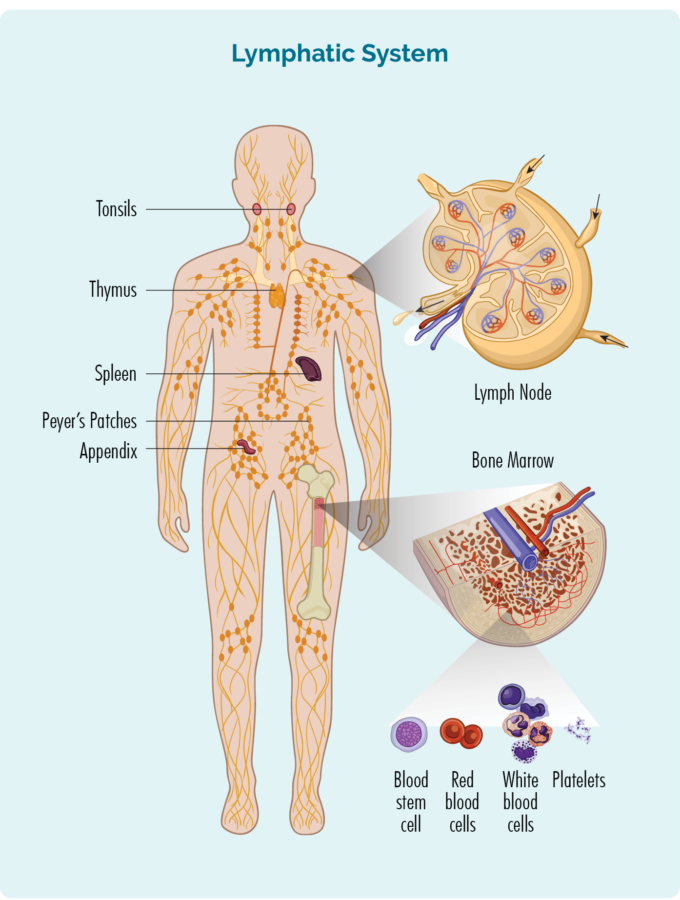
- T-cells are made from stem cells in our bone marrow, before moving out into our lymphatic system and thymus where they mature and live.
- Inside every T-cell is a nucleus that holds all of our DNA, which is made up of genes that tell our cells how to grow and work.
- They are usually resting in your thymus, lymph nodes or other parts of your lymphatic system, and only wake up and fight infection when other immune cells let them know there is an infection or disease to fight. When they wake up, T-cells can travel to any part of your body to fight the infection or disease.
- Some T-cells are responsible for “regulating” the immune response. This means that once an infection has been destroyed, the “Regulatory T-cells” tell other immune cells to “stand down” so they don’t keep fighting and cause harm to your good cells once the infection is gone.
- After fighting an infection or disease, some T-cells become “Memory T-cells” and they remember everything there is to know about the infection and how to fight it. That way, if you ever get the same infection or disease again, your immune system can fight it a lot more quickly and effectively.
What causes ATLL?
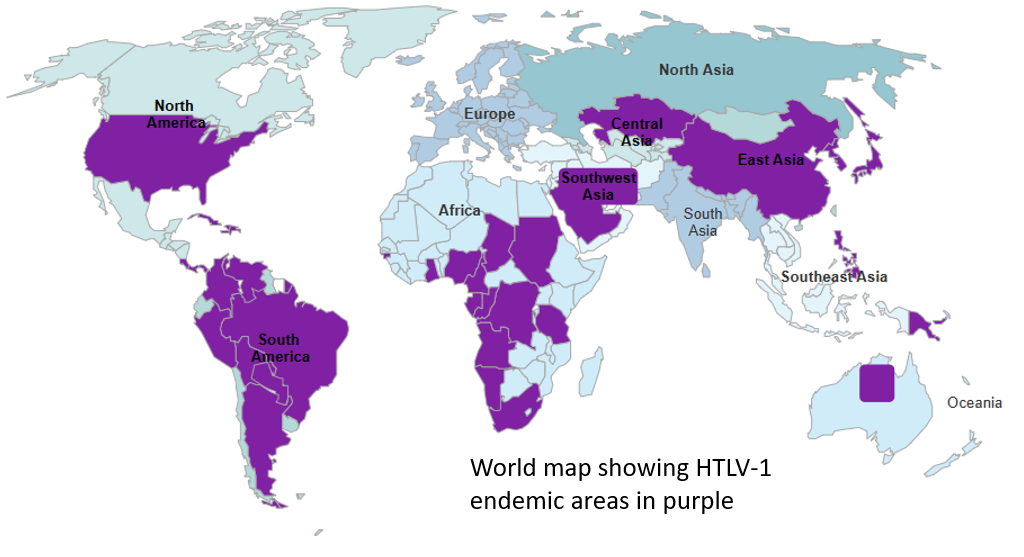
ATLL only occurs in people who have at some point had an infection with a rare virus called Human T-cell Lymphotropic Virus 1 (HTLV-1). Although the exact process is not fully understood, it seems that HTLV-1 causes changes in in your genes, causing them to give the wrong instructions on how the T-cells should grow and work. As a result the cancerous T-cells continue to multiply and make more cancerous T-cells.
However, most people with HTLV-1 never develop ATLL, so it is considered a risk factor, but not a cause. In fact, only about 1 in every 20 people with HTLV will develop ATLL. We don’t know why it develops in some people and not others.
Most people with HTLV-1 have been infected when they were infant being breastfed, or during childhood or early adulthood. In most cases, ATLL does not develop for 50 or more years after you first get HTLV-1.
For more information on causes and risk factors click here.
Endemic HTLV-1
Some viruses tend to be common in certain parts of the world, while not often found in other parts of the world. Where it is more common it is said to be endemic. You are more likely to be exposed to HTLV-1 if you have lived in a country or area where it is endemic.
If you have ever been diagnosed with HTLV-1 you should always use a barrier protection during sexual activity such as internal or external condoms with spermacide or a dental dam. This helps to protect your partner.
If you have a baby, you may be advised not to breastfeed and to use a good quality breastmilk substitute instead. If you want to have children, talk to your doctor about how to get pregnant while still protecting your partner and baby from HTLV-1.
You will also need to make sure if you are bleeding, that anyone helping you wears gloves and protects themselves from your blood. They should wash off any blood with running water and soap if they are exposed to your blood. They are more at risk of getting HTLV-1 if they have open sores or broken areas of skin and your blood gets on these broken areas. Never share needles of any type.
Symptoms of ATLL
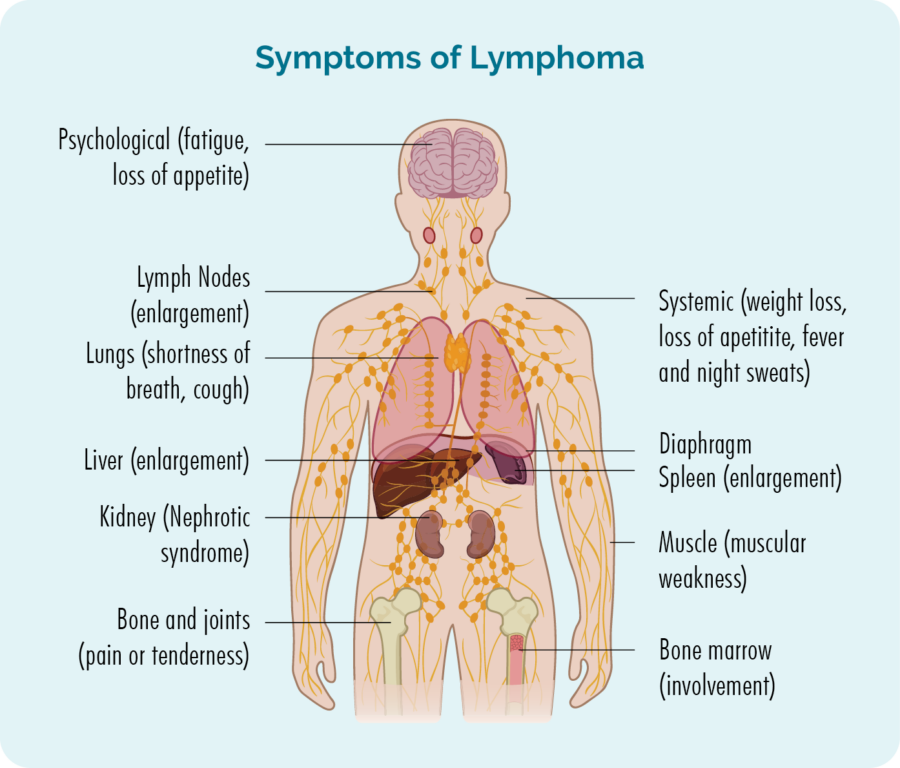
Symptoms of ATLL may be similar to symptoms of other types of lymphoma, or specific to the subtype of ATLL you have and the part of your body it is growing.
Common symptoms of many different subtypes of lymphoma can include:
- Fatigue
- Swollen lymph nodes that appear as lumps under your skin that you can see or feel.
- Aches and pains in your muscles and joints.
- Getting lots of infections, or difficulty getting over them.
- Itchy skin
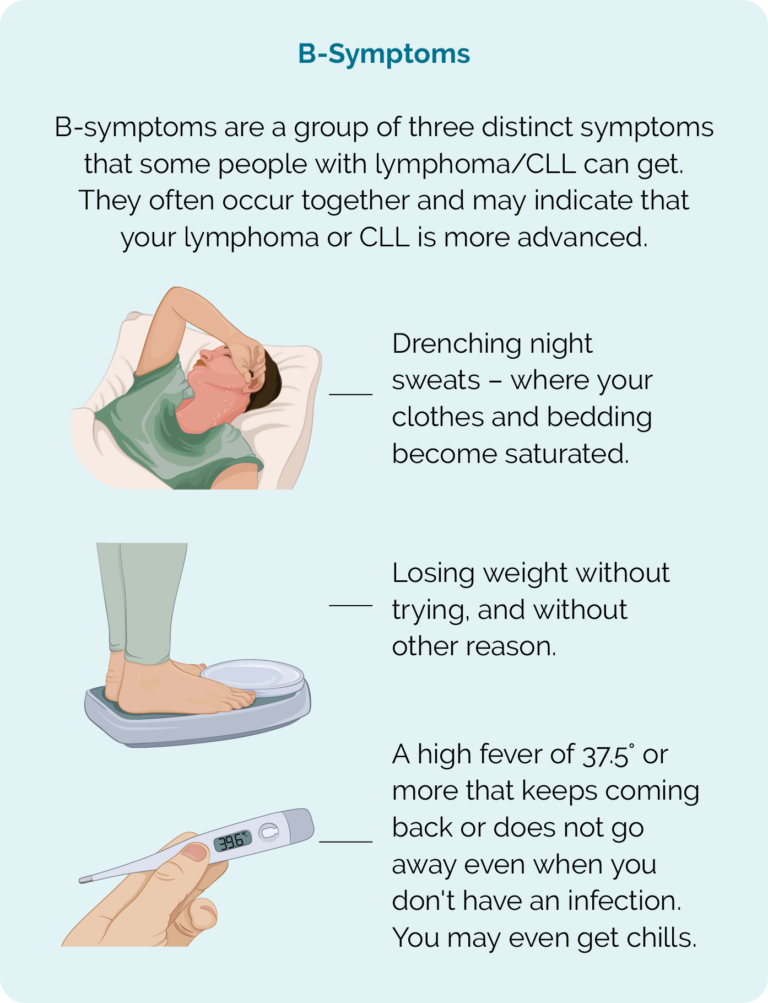
- B-symptoms
B-symptoms
Signs & Symptoms of different subtypes of ATLL | ||||
Symptoms | Acute ATLL | Lymphomatous ATLL | Chronic ATLL | Smoldering ATLL |
Lymphocytes in blood test | High to very high and abnormal appearance. | Usually normal. | A little high and few with abnormal appearance. | Normal, rarely some may appear abnormal. |
Lactate dehydrogenase (LDH) in blood test | High. | Usually normal. | Maybe a little high. | Normal. |
Calcium in blood test | High. | May be high or normal. | Normal. | Normal. |
Skin rash | Sometimes. | Sometimes. | Yes – red or darkened patches of skin. | Yes – skin lesions or little bumps on your skin. |
Swollen lymph nodes | Usually. | Yes. | Slight swelling. | No. |
Swollen liver and or spleen | Usually. | Often. | Mild. | No. |
Lymphoma cells in bone marrow | Sometimes. | Very rare. | No. | No. |
How is ATLL diagnosed and staged?
To diagnose lymphoma you will need a biopsy. The type of biopsy will depend on where your suspected lymphoma cells are in your body, and the symptoms you are having.
Types of biopsies
- Lymph node biopsy if you have swollen lymph nodes. Depending on where the lymph node is, you may have this with local anesthetic in the doctors’ rooms, or under general anesthetic in surgery if it is deep in your body.
- Biopsy of other tissue such as in your lungs or stomach if it is thought you may have lymphoma growing in these organs. This is usually done in surgery with a general anaesthetic.
- Bone marrow biopsy if you have increased white blood cell counts in your blood. This is usually done with local anesthetic, you may or may not have light sedation.
- Skin biopsy if you have a rash or lesions on your skin. This is usually done with local anesthetic.
You may need more than one biopsy. Fine needle biopsies are not recommended to diagnose lymphoma as they do provide enough tissue to be properly assessed. Instead, at a minimum you should have a core needle biopsy. This provides more tissue than fine needle biopsy. However, you may also need an excisional biopsy, which is where an entire lymph node is removed and checked in pathology.
Other tests you may need
You will also have blood tests to check your white blood cell count and calcium levels. You will also have a blood test to see if you have or have had HLTV-1. These are often be done together.
You may also have other tests such as CT scan, ultrasound or MRI. Sometimes you may have a biopsy done during theses scans so they can find, and make sure they biopsy the right areas.
Favorable (low) or Unfavorable (high) risk ATLL
ATLL is not staged in the same way other subtypes of lymphoma are staged. Instead ATLL is grouped into favorable or unfavorable risk. Favorable may also be called low risk, and unfavorable may also be called high risk.
Knowing your risk will help guide your doctor to recommend the best treatment options for you and give you the best advice.
Your risk will be unfavorable (high) if you have an aggressive ATLL or if you have chronic ATLL and your blood tests show:
- low albumin
- high lactate dehydrogenase (LDH)
- high blood urea nitrogen (BUN).
Waiting for results
Waiting for results can be a difficult time and it may help to talk to family, friends or a specialist nurse.
Subtypes of ATLL
There are 4 different subtypes of ATLL – 2 are aggressive and 2 are indolent. However, most people diagnsoed with ATLL will have an aggressive subtype, and about 1 in 4 people with indolent ATLL will progress to an aggressive type at some stage.
Click on the headings below to learn a little more about the different subtypes of ATLL and signs and symptoms you may get with specific subtypes. In addition to these, you may also get any of the general symptoms of lymphoma mentioned above.
Aggressive ATLLs
Acute means the ATLL starts and spreads quickly. It is considered an unfavorable or high risk ATLL.
You may get any of the symptoms listed above, but as well as those, other symptoms you may get with this subtype include:
- Extreme fatigue that comes on quickly and is not improved with rest or sleep.
- A rash on any part of your skin.
- Shortness of breath.
- Changes in your blood tests including high white blood cell count, high lymphocytes, calcium and lactate dehydrogenase (LDH) levels.
- Bone pain.
- Confusion.
- Irregular heartbeat.
- Constipation – can be severe.
- B-symptoms.
If you have any of the above signs and symptoms see your local doctor (GP) as soon as possible. They will need to assess you and organise tests and referrals for you. You will need to have treatment soon after being diagnosed with Acute ATLL.
This subtype is an aggressive and high risk ATLL. It is called lymphomatous because it mostly affects your lymphatic system, so the most common symptoms include:
- Swollen lymph nodes you can see or feel in your neck, underarms or groin. This is because these lymph nodes are closer to your skin so they can be more easily seen and felt. Swollen lymph nodes may be found in any part of your body with a CT or PET scan.
- Infections that are difficult to get over or keep coming back.
- Possible high levels of calcium and lactate dehydrogenase (LDH) in your blood tests.
- Rash or itchy skin
- Shortness of breath.
- Confusion.
If you have any of the above signs and symptoms see your local doctor (GP) as soon as possible. They will need to assess you and organise tests and referrals for you. You will need to have treatment soon after being diagnosed with lymphomatous ATLL.
Indolent ATLLs
Chronic ATLL can be high or low risk. It is usually slow growing so you may not notice any symptoms at first. Symptoms you do have may get worse over a long period of time. For this reason, many people put their symptoms down to other things like aging or stress. However, common signs and symptoms that you might get if you have chronic ATLL are:
- High levels of white blood cells on blood tests. These may gradually get higher over time.
- Swollen lymph nodes that increase in size over a long period of time.
- Enlarged spleen or liver.
- Rash or itching of your skin.
- Shortness of breath that gets worse over a long period of time (months to years).
- Fatigue.
- low albumin
- high lactate dehydrogenase (LDH)
- high blood urea nitrogen (BUN).
You may not need treatment straight away if you have low risk chronic ATLL, however this will depend on your signs and symptoms and if it is affecting your overall health.
You will normally start treatment soon after your diagnosis if you have high risk ATLL.
Smoldering ATLL is a very slow-growing subtype of lymphoma and is considered a low, or favorable risk ATLL.
You may not get any symptoms at all with this subtype. If you do, they are likely to be very mild and may include a rash or lesions (sores) on your skin that do not heal or go away. You may also experience shortness of breath which gets worse over a long period of time (months to years).
You may not need any treatment for smoldering ATLL, however if you do have skin lesions or rashes that are bothering you, you may only need treatment to improve these symptoms such as a steroid cream or radiation to the area affected.
Treatment of adult T-cell leukaemia-lymphoma (ATLL)
Multidisciplinary care
In many cases, your haematologist will meet with other haematologists and other health professionals to discuss your case. This is a great thing when you have a rare lymphoma because you get many different, very experienced people looking at your individual situation to determine the best way to help you, and make sure you get best the best treatment options and care.
You can also ask your haematologist to present your case at the Australasian Lymphoma T-cell Alliance meeting. This meeting brings together experts from around the country who are up to date with the latest research developments in rare T-cell lymphomas. They can advise your haematologist of any clinical trials or new treatment options available to you.
Before you start treatment
Before you start treatment there are some things you need to consider and prepare for. Having a list of things to do while waiting for treatment, can also help with the anxiety of waiting, because you will be actively working towards making things better for yourself.
Fertility
Many treatments can affect your fertility, making it more difficult or impossible to get pregnant, or get somebody else pregnant. If you are of child-bearing age, even if you are not thinking about having a family or extending your family just yet, you need to talk to your doctor about how to preserve your fertility, prevent unwanted pregnancies and prevent or manage early menopause or ovarian insufficiency.
Questions to ask your doctor
When you are first diagnosed, or starting treatment after a relapse, it can be difficult to think straight and know what questions to ask. But it’s important you have all the right information you need to make the decisions about your healthcare and know what to expect. Click on the link below to download Questions to ask your doctor.
Practical things you need to know and how to prepare
Having treatment is going to change your life and the lives of those closest to you for a while. It is important to know what to expect and prepare for. You also need to know what support is available to you. We have developed some tips on practical things you should know when you or a loved one has lymphoma. Click the link below for more information.
The doctors will take into consideration many factors about the lymphoma and your general health to decide when and what treatment is best for you. They will consider:
- The subtype of ATLL you have – and whether it is low or high risk.
- Any symptoms you have.
- Your age, past medical history, physical and emotional wellbeing.
- Whether you have ever had treatment for the ATLL in the past.
- Your eligibility to join a clinical trial.
- Your personal preferences after you’ve been given all the information you need to make a decision.
First-line treatment
The first time you have treatment for ATLL it is called first-line treatment. It is often given in cycles and you may have 4, or 6, or even 8 cycles of treatment as part of your first-line therapy. How many cycles you have will depend on the treatment protocol.
Common first-line treatments for high risk ATLL will usually include anti-viral medicine to control your HTLV-1 infection and may include chemotherapy treatment which may be any of the below.
- CHOP (cyclophosphamide, doxorubicin, vincristine and a steroid called prednisolone).
- CHOEP (cyclophosphamide, doxorubicin, vincristine, etoposide and a steroid called prednisolone).
- Bv-CHP (conjugated monoclonal antibody called Brentuximab vedotin, cyclophosphamide, doxorubicin and a steroid called prednisolone).
- Dose- adjusted EPOCH (etoposide, vincristine, doxorubicin, cyclophosphamide and a steroid called prednisolone).
- Hyper-CVAD (cyclophosphamide, vincristine, doxorubicin and a steroid called dexamethasone) alternating with high dose methotrexate and cytarabine.
- Stem cell transplant may be appropriate for some patients.
- Clinical trial participation.
If you have a low risk ATLL with mild or no symptoms, you may not need any chemotherapy at all. Instead you may have antiviral medicine to treat the HTLV-1 and any of the below treatment options.
- ‘Watch and wait’ (active monitoring).
- Steroid creams of lotions to improve symptoms of skin rashes and itching.
- Radiotherapy.
Relapsed or Refractory management of ATLL
ATLL usually responds well to Immunochemotherapy, but it often comes back (relapses), or in rare cases does not respond to initial treatment (refractory). When this happens, you may be eligible for different types of treatment or clinical trials.
Some treatments you may be offered are listed below however, with constant research and clinical trials improving treatments for people with relapsed and refractory lymphomas, you may be offered something different to the below.
- DHAP (dexamethasone, cytarabine and cisplatin)
- ESHAP (detoposide, methylprednisolone, cytarabine and cisplatin)
- GDP (gemcitabine, dexamethasone and cisplatin)
- ICE (ifosfamide, carboplatin and etoposide)
Finishing treatment
Finishing treatment can be exciting, or a very anxious time for you. It could even make you feel both excited and anxious. It is normal to feel many different emotions when you finish treatment. And, even if you coped well during treatment, you may find that once everything slows down and you have time to think about what you’ve been through, and how to get back to some kind of life that resembles life before treatment, you become overwhelmed.
You also have to deal with the emotions of others around you and their expectations. Many patients mention how hard it is when people around them expect them to be back to normal long before they are ready.
On the other hand, other patients have mentioned feeling like people around them hold on too tight and don’t let them get back to normal, because they are afraid something else might happen.
We have tips on what to expect, and how to manage emotions, and the expectations of other on our Finishing treatment webpage.
Follow up
You will continue to see your haematologist or oncologist regularly even after treatment ends. They will assess you for any ongoing side-effects from treatment, or any new side-effects that can happen months or even years after treatment ends. You can find more information about late effects by clicking the side effects of treatment link above.
They will also be assessing you signs for any signs of your lymphoma relapsing so that any needed treatment can start as soon as possible.
Your follow-up appointments may include any of the below:
- PET or CT scans and results
- Blood tests
- Physical examination of your lymph nodes
- Questions about how you are feeling, and adapting to life after treatment.
- Referrals for extra care if needed.
Summary
- ATLL is a very rare type of T-cell Non-Hodgkin Lymphoma. It can also be grouped as a subtype of Peripheral T-cell Lymphoma.
- ATLL has 4 different subtypes, and they may be classes a low or high risk depending on how aggressive it is, and how it is affecting your body.
- You may not have any symptoms, or only very mild symptoms if you have a low risk, indolent lymphoma.
- Report all new or worsening symptoms to your doctor for investigation, especially rashes that don’t go away, swollen lymph nodes or B-symptoms.
- A biopsy is needed to confirm a diagnosis of ATLL – sometimes more than one is needed.
- If you have a low risk ATLL you may not need treatment, but high risk ATLL will need treatment very quickly.
- ATLL can respond well to treatment, but often relapses needing more treatment.
- Ask your doctor about clinical trials you may be eligible for.
- You will continue to see your heamatologist or oncologist for regular check-ups even after treatment finishes.