Overview of Nodular Lymphocyte Predominant B-Cell Lymphoma (formerly NLPHL)
Nodular Lymphocyte Predominant B-cell Lymphoma (NLP-BCL) is a very rare subtype of lymphoma, which is a cancer of white blood cells called B-cell lymphocytes.
NLP-BCL is more common in people aged 30-50 years, but can affect people of any age. It is also more common in men than women.
It was previously considered a rarer subtype of Hodgkin Lymphoma which is identified through a type of cancerous cell called a Reed-Sternberg cell. However with more research, it has now been shown to be different to the Reed-Sternberg cell.
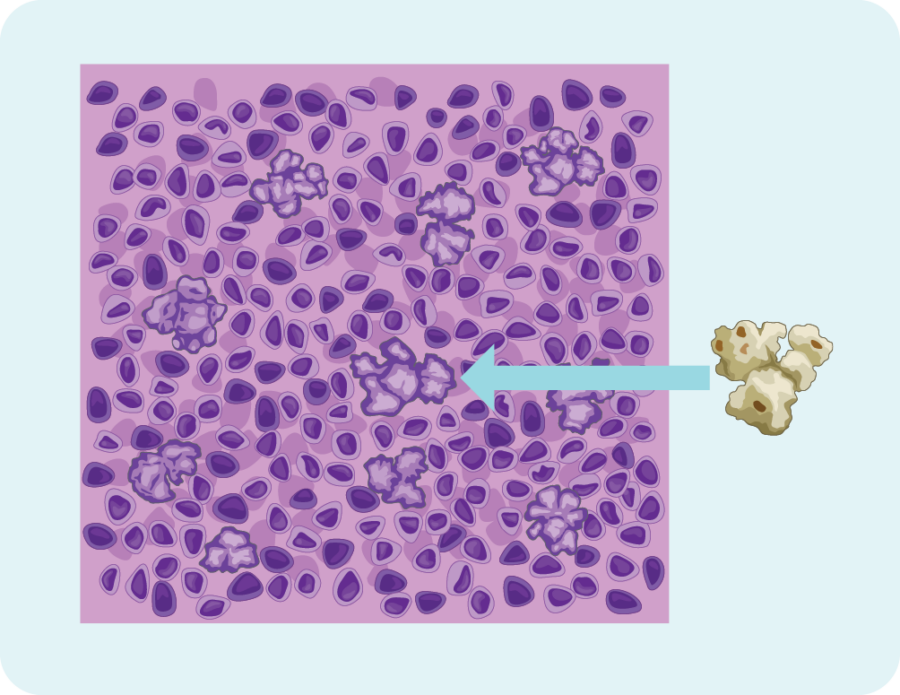
Firstly, they look bumpy (or nodular) a bit like a piece of popcorn.
CD20 Protein
NLPHL cells also have a protein on them called CD20. This is different from classical Hodgkin Lymphoma as no other subtype of Hodgkin Lymphoma has this protein.
However, CD20 is common on many types of B-cell Non-Hodgkin Lymphoma cells.
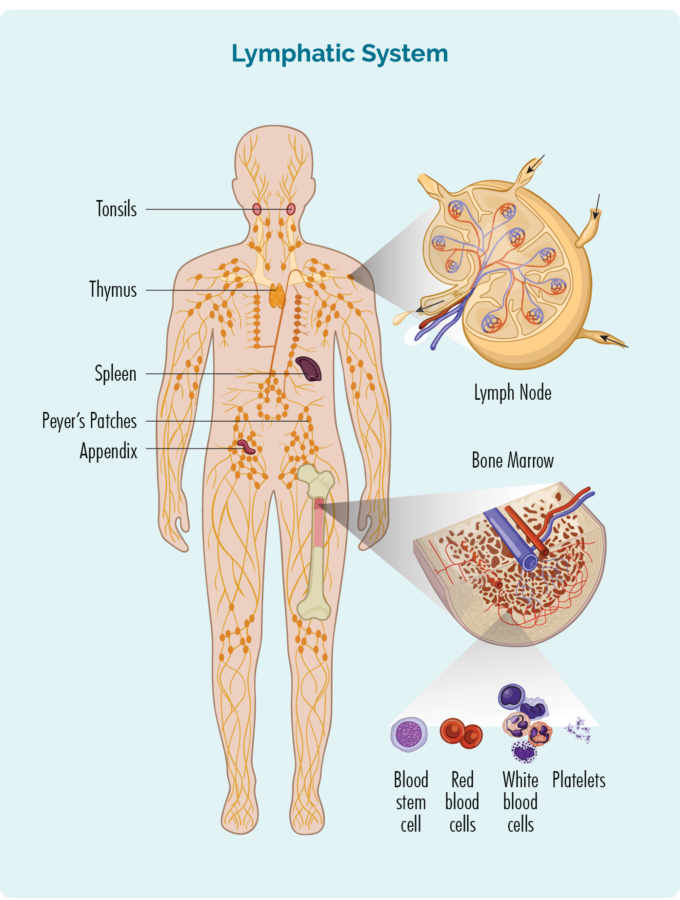
Understanding B-cell Lymphocytes
To understand NLP-BCL you need to know a bit about your B-Cell lymphocytes.
B-Cell lymphocytes:
- Are a type of white blood cell
- Fight infection and diseases to keep you healthy.
- Remember infections you had in the past, so if you get the same infection again, your body’s immune system can fight it more effectively and quickly.
- Are made in your bone marrow (the spongy part in the middle of your bones), but usually live in your spleen and your lymph nodes. Some live in your thymus and blood too.
- Can travel through your lymphatic system, to any part of your body to fight infection or disease.
NLP-BCL develops when some of your B-cells become cancerous. They grow uncontrollably, are abnormal, and do not die when they should.
When you have NLP-BCL your cancerous B-cell lymphocytes:
- Will not work as effectively to fight infections and disease.
- Look different to your healthy B-cells (They look like popcorn shaped Reed-Sternberg cells).
Symptoms of Nodular Lymphocytic Predominant B-cell Lymphoma (formerly NLPHL)
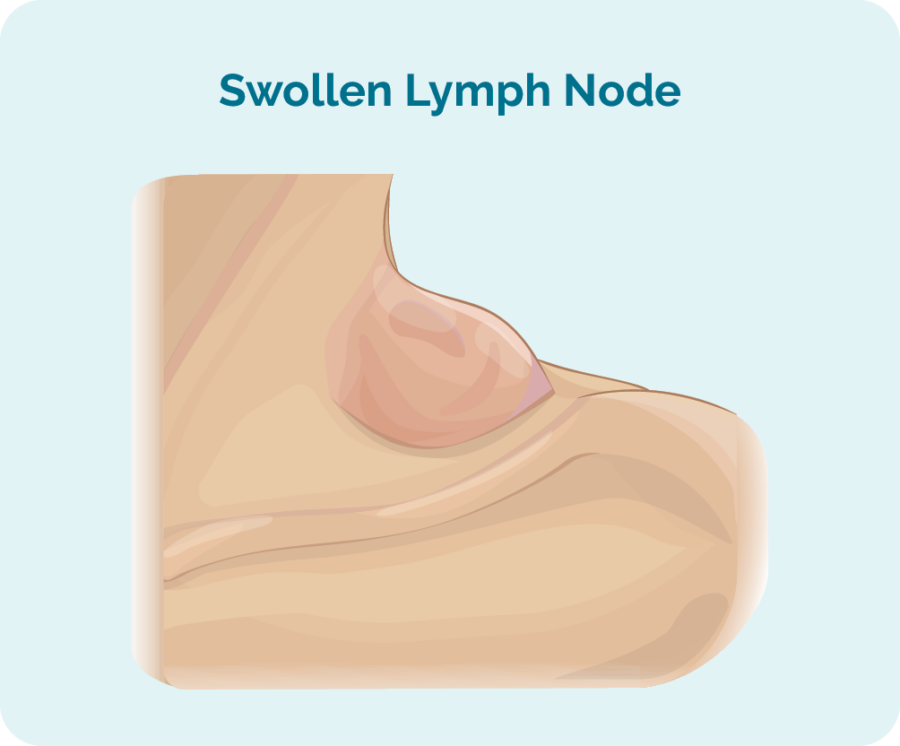
You may not get any symptoms of NLP-BCL because it grows very slowly. If you do get symptoms they may include the below symptoms.
- Swollen lymph node/s in your neck, armpit or groin.
- Fatigue – extreme tiredness that does not improve with rest or sleep.
- Feeling out of breathe for no reason.
- Bleeding or bruising more that usual.
- Infections that don’t go away or keep coming back.
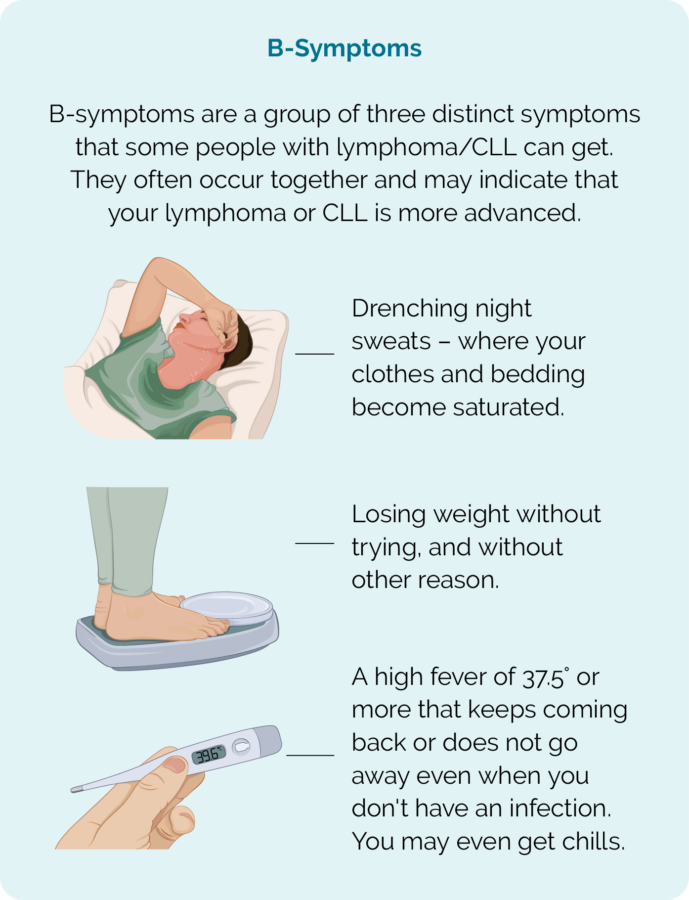
- B-symptoms.
How is NLP-BCL (formerly NLPHL) diagnosed
Diagnosing NLP-BCL can sometimes be difficult because it grows so slowly, often does not cause symptoms, and if you do have symptoms, they are often similar to symptoms you might get with other illnesses or conditions such as allergies, infection, stress, hormonal imbalances among others.
If your doctor thinks that you may have lymphoma, they will need to organise a number of important tests. These tests are needed to either confirm or rule out lymphoma as the cause for your symptoms.
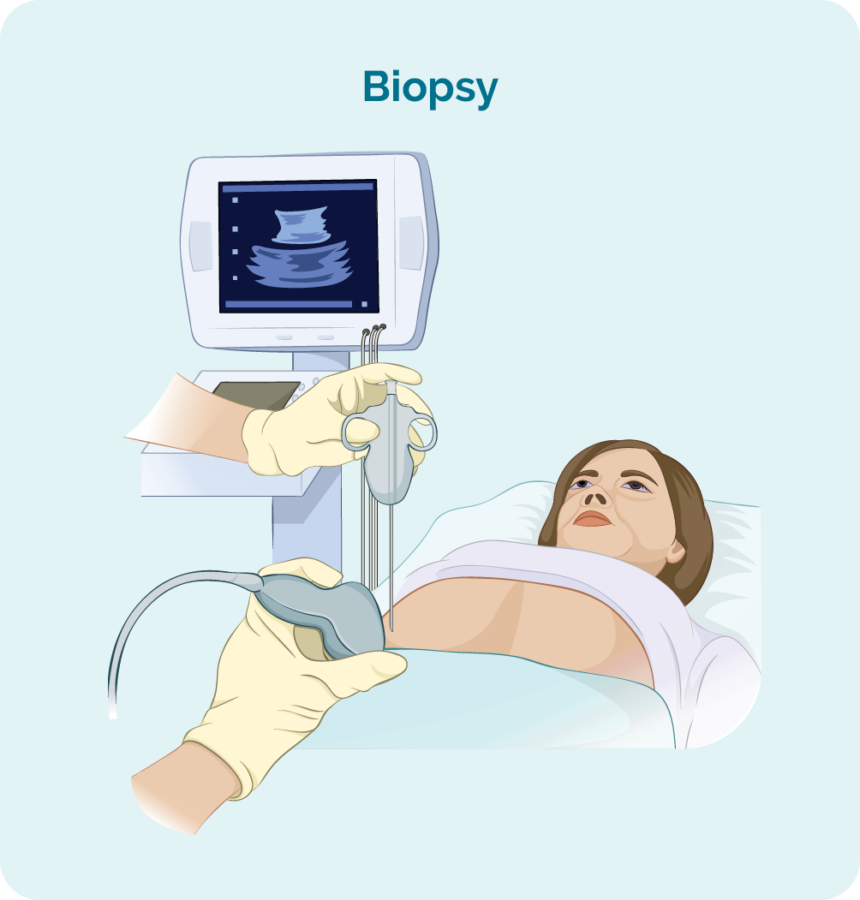
To diagnose NLP-BCL you will need a biopsy. A biopsy is a procedure to remove part, or all of an affected lymph node and/ or a bone marrow sample. The biopsy is then checked by scientists in a laboratory to see if there are changes that help the doctor diagnose NLP-BCL.
When you have a biopsy, you may have a local or general anaesthetic. This will depend on the type of biopsy and what part of your body it is taken from. There are different types of biopsies and you may need more than one to get the best sample.
Core or fine needle biopsy
Core or fine needle biopsies are taken to remove a sample of swollen lymph node or tumour to check for signs of NLP-BCL.
Your doctor will usually use a local anaesthetic to numb the area so you don’t feel any pain during the procedure, but you will be awake during this biopsy. They will then put a needle into the swollen lymph node or lump and remove a sample of tissue.
If your swollen lymph node or lump is deep inside your body the biopsy may be done with the help of ultrasound or specialised x-ray (imaging) guidance.
You might have a general anaesthetic for this (which puts you to sleep for a little while). You may also have a few stitches afterwards.
Core needle biopsies take a bigger sample than a fine needle biopsy.
Excisional node biopsy
Excisional node biopsies are done when your swollen lymph node or tumour are too deep in your body to be reached by a core or fine needle biopsy. You will have a general anaesthetic which will put you to sleep for a little while so you stay still, and feel no pain.
During this procedure, the surgeon will remove the whole lymph node or lump and send it to pathology for testing. You will have a small wound with a few stitches, and a dressing over the top. Stitches usually stay in for 7-10 days, but your doctor or nurse will give you instruction on how to care for the dressing, and when to return to have the stitches out.
Blood tests
Blood tests are taken when trying to diagnose your lymphoma, but also throughout your treatment to make sure your organs are working properly and can cope with our treatment.
Staging
Once your doctor gets the results from you blood tests and biopsies they will be able to tell you if you have NLP-BCL and start to make a plan for you. However, before they can make any suggestions about whether you need to start treatment or not, they will need more information about the stage and grade of your NLP-BCL.
Staging refers to how much of your body is affected by your lymphoma – or, how far it has spread from where it first started.
B-cells can travel to any part of your body. This means that lymphoma cells (the cancerous B-cells), can also travel to any part of your body. You will need to have more tests done to find this information. These tests are called staging tests and when you get results, you will find out if you have stage one (I), stage two (II), stage three (III) or stage four (IV) NLP-BCL.
Your stage of NLP-BCL will depend on:
- How many areas of your body have lymphoma
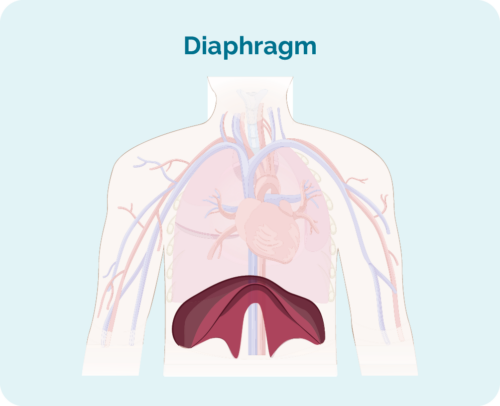
- Where the lymphoma is including if it is above, below or on both sides of your diaphragm (a large, dome-shaped muscle under the rib cage that separates the chest from your abdomen)
- Whether the lymphoma has spread to your bone marrow or other organs such as the liver, lungs, skin or bone.
Stages I and II are called ‘early or limited stage’ (involving a limited area of your body).
Stages III and IV are called ‘advanced stage’ (more widespread).
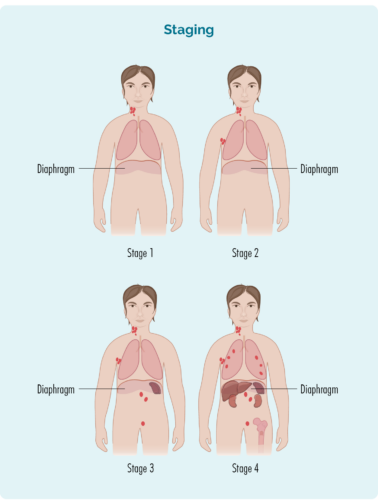
Stage 1 | one lymph node area is affected, either above or below the diaphragm* |
Stage 2 | two or more lymph node areas are affected on the same side of the diaphragm* |
Stage 3 | at least one lymph node area above and at least one lymph node area below the diaphragm* are affected |
Stage 4 | lymphoma is in multiple lymph nodes and has spread to other parts of the body (e.g. bones, lungs, liver) |
Extra staging information
Your doctor may also talk about your stage using a letter, such as A,B, E, X or S. These letters give more information about the symptoms you have or how your body is being affected by the lymphoma. All this information helps your doctor find the best treatment plan for you.
Letter | Meaning | Importance |
A or B |
|
|
E & X |
|
|
S |
|
(Your spleen is an organ in your lymphatic system that filters and cleans your blood, and is a place your B-cells rest and make antibodies) |
Tests for staging
To find out what stage you have, you may be asked to have some of the following staging tests:
Computed tomography (CT) scan
These scans takes pictures of the inside of your chest, abdomen or pelvis. They provide detailed pictures that provide more information than a standard X-ray.
Positron emission tomography (PET) scan
This is a scan that takes pictures of the inside of your whole body. You will be given and needle with some medicine that cancerous cells – such as lymphoma cells absorb. The medicine that helps the PET scan identify where the lymphoma is and the size and shape by highlighting areas with lymphoma cells. These areas are sometimes called “hot”.
Lumbar puncture
A lumbar puncture is a procedure done to check if you have any lymphoma in your central nervous system (CNS), which includes your brain, spinal cord and an area around your eyes. You will need to say very still during the procedure, so babies and children may have a general anaesthetic to put them to sleep for a little while the procedure is done. Most adults will only need a local anaesthetic for the procedure to numb the area.
Your doctor will put a needle into your back, and take out a little bit of fluid called “cerebral spinal fluid” (CSF) from around your spinal cord. CSF is a fluid that acts a bit like a shock absorber to your CNS. It also carries different proteins and infection fighting immune cells such as lymphocytes to protect your brain and spinal cord. CSF can also help drain any extra fluid you may have in your brain or around your spinal cord to prevent swelling in those areas.
The CSF sample will then be sent to pathology and checked for any signs of lymphoma.
Bone marrow biopsy
- Bone marrow aspirate (BMA): this test takes a small amount of the liquid found in the bone marrow space.
- Bone marrow aspirate trephine (BMAT): this test takes a small sample of the bone marrow tissue.
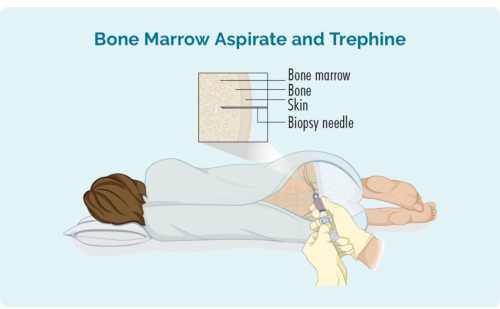
The samples are then sent to pathology where they are checked for signs of lymphoma.
The process for bone marrow biopsies can differ depending on where you are having your treatment, but will usually include a local anaesthetic to numb the area.
In some hospitals, you may be given light sedation which helps you to relax and can stop you from remembering the procedure. However many people do not need this and may instead have a “green whistle” to suck on. This green whistle has a pain killing medication in it (called Penthrox or methoxyflurane), that you use as needed throughout the procedure.
Make sure you ask your doctor what is available to make you more comfortable during the procedure, and talk to them about what you think will be the best option for you.
Your lymphoma cells have a different growth pattern, and look different to normal cells. The grade of your lymphoma is how quickly your lymphoma cells are growing, which affects the way look under a microscope. The grades are Grades 1-4 (low, intermediate, high). If you have a higher grade lymphoma, your lymphoma cells will look the most different from normal cells, because they are growing too quickly to develop properly. An overview of the grades is below.
- G1 – low grade – your cells look close to normal, and they grow and spread slowly.
- G2 – intermediate grade – your cells are starting to look different but some normal cells exist, and they grow and spread at a moderate rate.
- G3 – high grade – your cells look fairly different with a few normal cells, and they grow and spread faster.
- G4 – high grade – your cells look most different to normal, and they grow and spread the fastest.
All this information adds to the whole picture your doctor builds to help decide the best type of the treatment for you.
It is important that you talk to your doctor about your own risk factors so you can have clear idea of what to expect from your treatments.
It is important to note that lymphoma is what is known as a systemic cancer. This means it can often spread throughout your lymphatic system and into any part of your body. It is not uncommon to be diagnosed with an advanced stage of lymphoma, but unlike advanced stage solid tumour cancers, such as bowel or lung cancer even advanced lymphoma’s can often be cured or put into remission with treatment.
NLP-BCL is a highly treatable lymphoma with standard first-line treatment and about 9 out of every 10 (90%) of people with NLP-BCL will be cured or have a long remission period (10 years or longer at a time) after treatment.
Treatment for Nodular Lymphocyte Predominant B-cell Lymphoma (formerly NLPHL)
Doctors take into consideration many factors about the lymphoma and the patient’s general health to decide when and what treatment is required.
This is based on:
- The stage of lymphoma
- Symptoms (including the size and location of the lymphoma)
- How the lymphoma is affecting the body
- Age
- Past medical history & general health
- Current physical and mental wellbeing
- Patient preferences
If treatment is needed, the patient’s type and severity of the symptoms, age, overall health and degree of the thickness of the blood, will help determine which treatment is selected.
Before you start treatment
Fertility
Some treatments for lymphoma can affect your fertility, making it harder to get pregnant, or get someone else pregnant. This can happen with several different types of anticancer treatments including:
- chemotherapy
- radiotherapy (when it is too your pelvis)
- antibody therapies (monoclonal antibodies and immune checkpoint inhibitors)
- stem cell transplants (because of the high-dose chemotherapy you will need before the transplant).
Make sure you have all the following information before you start your treatment.
- The name of your treatment
- What are the common and possible side effects for the treatment
- What side effects do you need to report to your medical team
- What are the contact numbers, and where to go if your have an emergency 7 days a week and 24 hours per day.
First-line treatment
The first time you have treatment for your lymphoma it is called first-line treatment. Depending on your individual circumstances, first-line treatment can include any of the following:
Early Stage NLP-BCL without B symptoms
Radiotherapy alone
Surgery followed by radiotherapy
Surgery alone
Early Stage NLP-BCL with B symptoms
Chemotherapy and monoclonal antibody *CVP-R x 2-3 cycles followed by radiotherapy
Chemotherapy and monoclonal antibody CVP-R x 6 cycles
Advanced Stage NLP-BCL
Chemotherapy and monoclonal antibody *CHOP-R x 6 cycles
Chemotherapy and monoclonal antibody *ABVD-R x 6 cycles
Chemotherapy and monoclonal antibody CVP-R x 6 cycles
- CVP-R (cyclophosphamide, vincristine, prednisolone and rituximab)
- CHOP-R (cyclophosphamide, doxorubicin, vincristine, prednisolone and rituximab)
- ABVD-R (doxorubicin, bleomycin, vinblastine, dacarbazine and rituximab)
Common side effects of treatment
Side effects of your treatment will depend on the type of treatment you are having, and in some cases the location of your lymphoma. Your treating doctor and/or cancer nurse can explain the specific side effects of your treatment before you start. However, some of the more common side effects of anticancer treatments may include:
- Anaemia (low red blood cells carry oxygen around the body)
- Thrombocytopenia (low platelets that help bleeding and clotting)
- Neutropenia (low white blood cells help with immunity)
- Nausea and vomiting
- Bowel problems such as constipation or diarrhoea
- Fatigue (tiredness or lack of energy
You can learn more about these side-effects by clicking the link below.
Second-line treatment
Most people respond really well to first-line treatment and never need treatment again. However, in rare cases, your lymphoma may not respond to your first-line treatment as well as hoped. When this happens, your lymphoma is called refractory.
In other cases, your first-line treatment may put you into remission (where there are no signs of lymphoma left in your body) but it may come back at after some time (relapse).
If you have refractory or relapsed NLP-BCL you will need to start a new treatment. This new treatment is called Second-line treatment.
Second-line treatment may include:
- Different chemotherapy medicines
- Monoclonal antibodies
- Stem cell transplant
- Clinical trials
Clinical Trials
It is recommended that anytime you need to start new treatments you ask your doctor about clinical trials you may be eligible for. Clinical trials are important to find new medicines, or combinations of medicines to improve treatment of Lymphoma in the future.
They can also offer you a chance to try a new medicine, combination of medicines or other treatments that you would not be able to get outside of the trial. If you are interested in participating in a clinical trial, ask your doctor what clinical trials you are eligible for.
There are many treatments and new treatment combinations that are currently being tested in clinical trials around the world for patients with both newly diagnosed and relapsed lymphoma.
Prognosis & Follow-up care
Prognosis is the term used to describe the likely path of your disease, how it will respond to treatment and how you will do during and after treatment.
There are many factors that contribute to your prognosis and it is not possible to give an overall statement about prognosis. However, NLP-BCL often responds very well to treatment and many patients with this cancer can be cured – meaning after treatment, there is no sign of lymphoma in your body.
Factors that can impact prognosis
Some factors that may impact your prognosis include:
- You age and overall health at time of diagnosis.
- How you respond to treatment.
- What if any genetic mutations you have.
If you would like to know more about your own prognosis, please talk with your specialist haematologist or oncologist. They will be able to explain your risk factors and prognosis to you.
Follow-up care
When you finish your treatment your haematologist will still want to see you regularly. You will have regular check-ups including blood tests and scans. How often you have these tests will depend on your individual circumstance and your haematologist will be able to tell you how often they want to see you.
It can be an exciting time or a stressful time when you finish treatment – sometimes both. There is no right or wrong way to feel. But it is important to talk about your feelings and what you need with your loved ones.
Support is available if you are having a difficult time coping with the end of treatment. Talk to your treating team – your haematologist or specialist cancer nurse as they may be able to refer you for counselling services within the hospital. Your local doctor (general practitioner – GP) can also help with this.
Lymphoma Care Nurses
You can also give one of our Lymphoma Care Nurses or email. Just click on the “Contact Us” button at the bottom of the screen for contact details.
Survivorship - Living with, and after cancer
A healthy lifestyle, or some positive lifestyle changes after treatment can be a great help to your recovery. There are many things you can do to help you live well with NLP-BCL.
Many people find that after a cancer diagnosis, or treatment, that their goals and priorities in life change. Getting to know what your ‘new normal’ is can take time and be frustrating. Expectations of your family and friends may be different to yours. You may feel isolated, fatigued or any number of different emotions that can change each day.
The main goals after treatment for your NLP-BCL is to get back to life and:
- be as active as possible in your work, family, and other life roles
- lessen the side effects and symptoms of the cancer and its treatment
- identify and manage any late side effects
- help keep you as independent as possible
- improve your quality of life and maintain good mental health
Different types of cancer rehabilitation may be recommended to you. This could mean any of a wide range of services such as:
- physical therapy, pain management
- nutritional and exercise planning
- emotional, career and financial counselling.
Sometimes a side effect from treatment may continue or develop months or years after treatment has completed. This is called a late effect. It is important to report any new or worsening symptoms to your medical team.
Summary
- Nodular Lymphocyte Predominant B-cell Lymphoma (NLP-BCL) was previously called Nodular Lymphocyte Predominant Hodgkin Lymphoma (NLPHL), but was renamed by the World Health Organisation in 2022, due to differences between this subtype of lymphoma and classical subtypes of Hodgkin Lymphoma.
- NLP-BCL is a subtype of lymphoma identified when lymphoma cells are CD20 positive, popcorn looking, Reed-Sternberg cells.
- Not everyone with NLP-BCL will have symptoms, but a swollen lymph node that does not go away is the most common symptoms.
- B-symptoms and other lasting symptoms should be reported to your doctor for investigation.
- NLP-BCL may or may not need treatment, and usually responds well to treatment when given.
- In some rare cases NLP-BCL may be refractory or relapse, so you may need treatment more than once.
- Talk to your doctor about preserving your fertility before starting treatments.
- Reach out the the lymphoma care nurses by clicking the “contact us” button at the bottom of this screen.

