Overview of Waldenstrom’s Macroglobulinemia (WM)
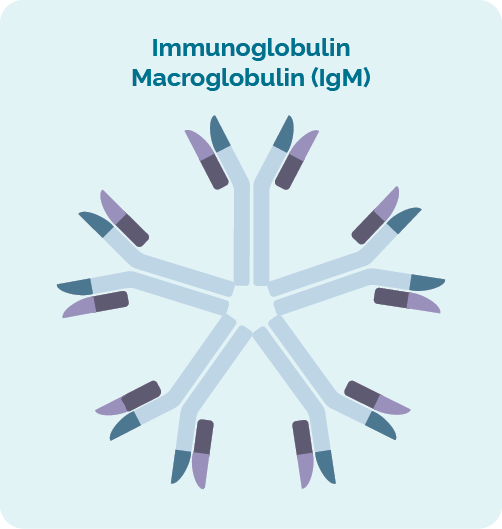
Immunoglobulin Macroglobulinemia (IgM)
Waldenstrom’s Macroglobulinemia starts when cancerous white blood cells called B-cell lymphocytes make too much of an Immunoglobulin called Macroglobulin (IgM).
Immunoglobulins are a type of protein that are also called antibodies. We have different types of immunoglobulins, but IgM is the biggest, and the first one made whenever we get an infection.
Immunoglobulins look like the letter the Y and IgM looks like five Y’s all joined together. Their job is to fight infection and diseased cells to keep us healthy. When you have too much IgM in your blood, your blood can become very thick – or viscous.
The thickened blood is referred to as being hyperviscous or as hyperviscosity. However, some cancerous B-cells and the extra IgM can also be found in your lymph nodes, causing them to swell up and cause a lump to form under your skin.
Waldenstrom is the name of the Doctor that first discovered this disease and Macroglobulinemia means there is too much Macroglobulin in your blood or bone marrow.
Plasma cells
The B-cell lymphocytes that make immunoglobulins are called “Plasma cells” and they are the most mature form of the B-cell lymphocyte. Most cancers of Plasma cells are called myeloma but in WM, the B-cell becomes cancerous just before it matures into the Plasma cell. So it has features of both lymphoma and myeloma, and causes uncontrolled production of the IgM protein.
Who gets Waldenstrom’s Macroglobulinemia (WM)?
Waldenstrom’s Macroglobulinemia (WM) is more common in men than women and usually happens after the age of 65 years.
We don’t know what causes WM, but if you’ve had certain infections, inflammatory conditions or autoimmune diseases such as Sjogren syndrome you may have a higher risk of getting it.
In some cases, if you have a family member with WM you may also be at an increased risk. However, most people with WM have no family members with it.
Cytogenetics in WM
There are two main genetic factors that can be affected when you have WM. To find if you have genetic factors that are involved in your disease, you will need to have cytogenetic tests done.
Cytogenetic Tests
Cytogenetics tests are done on your blood and biopsies to look for changes in your chromosomes or genes. We usually have 23 pairs of chromosomes, but if you have WM your chromosomes may look a little different.
Chromosomes & DNA
All of the cells of our body (except for red blood cells) have a nucleus, which is where our chromosomes are found. Chromosomes inside cells are long strands of DNA (deoxyribonucleic acid). DNA is the main part of the chromosome that holds the cell’s instructions, and this part is called a gene. Each DNA strand is made up of lots of genes.
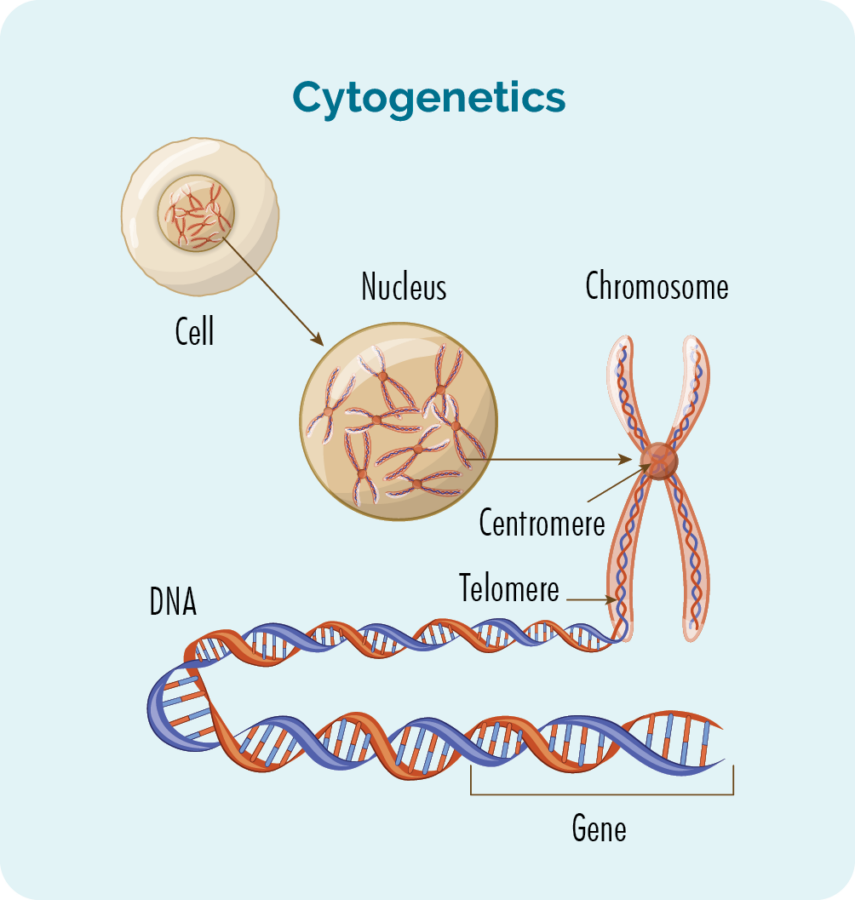
Genes
Genes tell the proteins and cells in your body how to look or act. If there is a change (variation or mutation) in these chromosomes or genes, your proteins and cells will not work properly, and you can develop different diseases. With WM these changes can change the way your B-cell lymphocytes develop and grow, causing them to become cancerous and make too much IgM.
Genes are usually named with a group of letters and numbers. The most likely to have a mutation when you have WM include:
- MYD88 gene – This gene is mutated in about 9 out of every 10 people with WM
- CXCR4 gene – This gene is mutated in about 1 in every 3 people with WM.
It’s important to know if you have these gene mutations, as some treatments work differently depending on the type of genetic mutations you have.
Symptoms of WM
About 1 in 4 people with WM have no symptoms, so being told you have it may come as real shock if you’ve just had blood tests or scans for some other reason.
If you do get symptoms they may be caused by hyperviscosity – Remember that’s when your blood gets too thick from all the extra IgM proteins in your blood.
Symptoms of hyperviscosity can include:
- headaches
- changes to your eye sight or hearing
- fatigue – extreme tiredness and weakness not improved with rest or sleep
- high blood pressure or changes to your heart rhythm
- muscle cramps
- confusion
- seizures
- low blood counts.
Low blood counts can happen if you have hyperviscosity because the increase of cancerous cells and IgM in your blood and bone marrow crowds out your good cells, making it hard for your body to make new blood cells. The blood cells affected can included your red cells, white cells and platelets.
Red cells have a protein called haemoglobin (Hb) on them that carry oxygen around your body. If they are low you can get:
- dizzy
- confused
- changes to your vision
- fatigue
- short of breath.
White cells – we have different types of white blood cells. They include our B-cell lymphocytes and other lymphocytes, but also others called neutrophils, eosinophils, basophils, mast cells and Plasma cells. These are all responsible for fighting infection and disease. One of the main ones those are the neutrophils, and when these are low it is called neutropenia. If you are neutropenic you can:
- get infections that don’t go away
- get Infections that keep coming back
- have difficulty healing if you hurt yourself
- get a high temperature or chills.
When you are neutropenic infection can get out of control very quickly. It is important you contact your doctor if you experience these symptoms, because you may need to be started on antibiotics very quickly.
Platelets – are the cells that help our blood to clot when we bump or cut ourselves. Another name for platelets is thrombocytes, so when your platelets are too low it is called thrombocytopenia. If you have thrombocytopenia you can:
- bruise more easily than usual
- bleed more easily or for longer than usual
- develop a spotty rash – which is little bits of blood leaking out under our skin
- bleed from our nose, gums, or when we go to the toilet.
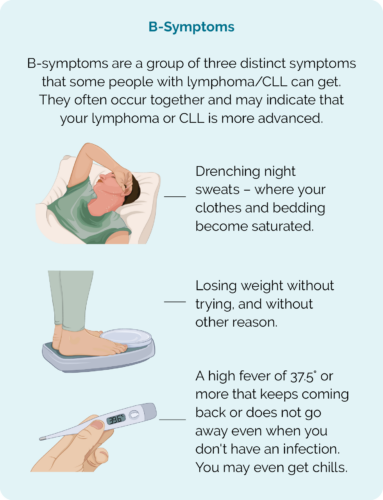
B-symptoms
You can also get B-symptoms with WM. It is often a sign that you need to start treatment because they can happen when the WM is actively growing. They include the three symptoms in the picture below.
Very rarely, in about 1 out of every 100 people with WM, cancerous lymphocytes and plasma cells build up in your central nervous system (brain and spinal cord). This is called ‘Bing-Neel syndrome’. It is rare and may cause headaches, fits – seizures, confusion or abnormal movements.
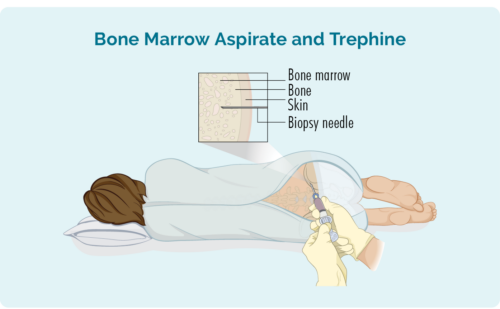
Diagnosis and staging of WM
You may be diagnosed with WM after you have a blood test. But your doctor will want to do some more tests to confirm this and look at what parts of your body are affected. Some of these tests will include:
- More blood tests
- Bone marrow biopsy (aspirate and trephine)
- Computed tomography (CT) scan (only if your doctor thinks your WM is affecting your lymph nodes)
- Tests on your heart, liver and kidneys
Learn about the Management of Waldenstrom's Macrobulinemia with Professor Judith Trotman, Consultant Haematologist - Concord Hospital
Treatment for Waldenstrom’s Macroglobulinemia (WM)
Once your doctor has all the information from your tests and scans, they will sit down with you and talk to you about the best way to manage you WM. In many cases they may suggest you do not need any treatment and instead, start you on a Watch & Wait management plan. Watch & Wait is used for many types of indolent lymphomas, because sometimes the risks can outweigh the benefits of treatment. You can learn more about Watch & Wait by clicking the link below.
If you are getting symptoms, or if your IgM levels are 60g/dL or above, you may need to start treatment. If you do need to start treatment, your doctors will take into consideration many factors about you and your WM to decide which treatment will be best for you.
Some of these include:
- Your IgM level.
- Any symptoms you are getting.
- If any of your organs are being affected by the increased IgM levels.
- Your age and overall well-being.
- If you have and other medical conditions.
- Your own preferences once you have all the information you need to make an informed decision.
Before you start treatment
Before you start treatment, let your doctor know if you are hoping to have children in the future. Many anti-cancer treatments can affect your fertility, or cause harm to unborn babies, so it is important to talk to your doctor about these things. In some cases, they may be able to organise some extra treatments to increase your chances of getting pregnant, or getting someone else pregnant in the future.
There are also other things you should talk to your doctor about, but it can be hard to know what questions to ask when you are first diagnosed. To help guide your conversation we have put together some questions you may like to ask. Click on the link below to download our Questions to ask your doctor.
Standard first-line treatment
The first-time you start treatment for WM it is called first-line treatment may include:
- DRC – includes dexamethasone (a steroid), rituximab (a monoclonal antibody) and a tablet called cyclophosphamide (chemotherapy).
- R-Benda (or BR) includes rituximab (a monoclonal antibody) and bendamustine (a chemotherapy).
- Rituximab and Zanubrutinib (Brukinsa™) – a targeted therapy called a BTK inhibitor.
- Zanubrutinib (Brukinsa™) only- (if chemo-immunotherapy not suitable)
- Clinical trial.
- Plasmapheresis (also called plasma exchange), if your blood is too thick from high IgM levels.
- Blood transfusions for low platelets and low red blood cells.
- IntraVenous ImmunoGlobulin replacement therapy (IVIG) if your immunoglobulin (antibody) levels are too low or you are getting frequent infections.
Common side effects of treatment
The side-effects you will depend on the type of treatment you get. It is important that you let your doctor know about new side-effects or symptoms you get during and after your treatment.
Some of the more common side effects of treatment may include:
- Neutropenia – this is when your white blood cells called neutrophils are too low and can result in you getting infections. If you get a temperature of 38° (degrees Celsius) or above, chills and shakes – called rigors, or you feel unwell, you need to contact your doctor immediately or attend the nearest emergency department.
- Thrombocytopenia – is when your platelets levels are too low. Platelets help our blood to clot to stop us from bleeding or bruising too much. If you notice you are bleeding or bruising more easily then normal, or if you get a reddish or puple spotty rash, contact your doctor to let them know.
- Anaemia is when you have low red blood cells. These cells transport oxygen around your body so when these are low you can feel tired, dizzy, weak, have changes to your vision or feel short of breath. Let your doctor know if you have any of these symptoms.
- Nausea and vomiting – make sure you are taking your anti-sickness medications the way your doctor or pharmacist told you to and let them know if it is not working. Other things you could try is and food or drink with ginger in it, eating small bland foods and avoiding spicy foods. Sometimes using plastic or wooden knives and forks instead of metal ones can also help.
- Bowel problems (constipation or diarrhea). It’s important to talk to your doctor about any changes to how your bowels are working. There are some medications you can use for diarrhea or constipation but this will depend on the type of treatment you are having and the cause of your bowel problems.
- Fatigue – is tiredness or a lack of energy that doesn’t get better after a rest or sleep. It can happen because of as a symptom of your WM, of as a side-effect of your treatment or for other reasons. Talk to your doctor if you are expereince that is not improving.
- Flu-like symptoms – includes fevers, muscle and joint pains, fatigue, rash, or generally feeling unwell. This can be a side-effect many anticancer treatments and you should let your doctor know if you’re getting these.
Follow-up care
Once treatment has completed, your doctor will continue to monitor your IgM levels to review how well the treatment has worked and know if and when you may need more treatment. The IgM levels will show the doctor if there has been a:
- Complete response – CR or no signs of abnormal IgM levels remain, or a
- Very good partial response (VGPR) – where there has been a very good response and a your IgM levels have decreased by 90%, or a
- Partial response – PR or there is has been a decrease in IgM levels of 50% (half) of what is before you started treatment.
Other ways to assess your response to treatment
However, it is important to note that sometimes the aim of treatment is to help improve your symptoms such as fatigue caused by anaemia (low red blood cells or haemoglobin), or symptoms caused by autoimmune responses as a result of the high IgM levels. So your doctor may be more concerned about these symptoms and how they have improved, rather than the IgM levels.
Your IgM levels are important though if you are considering going on to a clinical trial. This is because your IgM levels, and changes to it with the trial treatment will be an important part of the trial data. It will help researchers identify if the clinical trial treatment is better than current standard treatments at managing your WM.
Long-term follow-up
If all goes well regular follow-up appointments will be made for every 3-6 months to monitor the below:
- Review the effectiveness of the treatment
- Monitor any ongoing side effects from the treatment
- Monitor for any late effects from treatment over time
- Monitor signs of the lymphoma relapsing
These appointments are also important so that the patient can raise any concerns that they may need to discuss with the medical team. A physical examination and blood tests are also standard tests for these appointments. Apart from immediately after treatment to review how the treatment has worked, scans are not usually done unless there is a reason for them. For some patient’s appointments may become less frequent over time
Prognosis for Waldenstrom’s Macroglobulinemia (WM)
Like most indolent subtypes of lymphoma, WM cannot be cured. Instead, if you need treatment the aim will not be to cure but to manage the disease. This means keeping your IgM levels at a level that does not cause damage to your organs, thicken your blood too much, or cause you to get uncomfortable symptoms.
Most people get a really good response from treatment, and go into remission, however because we cannot cure WM, it is common for it to come back (relapse) and for you to need more treatment at a later time. For some people, it may be months, and for others it could be years before you need more treatment.
Rarely, WM can change (transform) into a faster growing (high-grade) type of lymphoma, usually Diffuse Large B-Cell Lymphoma (DLBCL).
Relapsed or refractory (RR) WM
Most people having treatment for WM respond well to the treatment and go into remission. But in some people the lymphoma comes back (relapses), or in rare cases does not respond to the first-line treatment (refractory). If you have RR WM, you may need to start treatment again, or start a new treatment. This next lot of treatment will be called second-line treatment.
Before you start the next treatment, your doctor will consider several things while trying to find the best treatment for you including:
- How long it has been since your last treatment and how well it worked for you.
- how long you have been in remission for.
- Side-effects you had with previous treatments.
- Your age and general well-being.
- Your preferences once you have all the right information to make the best choice for you.
Depending on your individual circumstance. You may be offered the same treatment you had before if it worked well, and you have been in remission for several years. You may also be offered one of the other treatments listed above. If you need to start second-line treatment, it is a good idea to ask your doctor about any clinical trials you may be eligible for.
Some treatment options you may be offered for RR WM
- Rituximab with or without chemotherapy
- Rituximab with zanubrutinib (Brukinsa™)
- Zanubrutinib (Brukinsa™) alone
- Plasmapheresis
- Clinical trial.
Clinical Trials – Treatments under investigation
There are new clinical trials starting all the time and it is a good idea to keep up to date with what new treatments are being tested to improve the treatment, or quality of life for people with WM. If you are interested in participating in a clinical trial, you can ask your doctor if you meet the inclusion criteria for the study.
Below are links to websites where you can search for clinical trials you may be eligible for. Try searching for:
- Waldenstroms Or Waldenstrom’s
- Waldenstrom’s Macroglobulinemia
- WM
Clinical trial websites
Health and wellbeing
A healthy lifestyle, or some positive lifestyle changes after treatment can be a great help after you finish treatment. Making small changes such as eating well and increasing your overall fitness can improve your health and wellbeing and help your body to recover. There are many self-care strategies that can help during your recovery. Click on the link for more tips on living well.
Summary
- Waldenstrom’s Macroglobulinemia (WM) is a cancer of your white blood cells called B-cell lymphocytes.
- The cancerous B-cell lymphocytes make too much of a protein called Immunoglobulin Macroglobulin (IgM), which can make your blood to thick and prevent your body making other health blood cells.
- Many people do not get any symptoms, but symptoms can happen as the WM gets more advanced or as your IgM levels increase.
- Let your doctor know if you are getting any of the symptoms listed above, including B-symptoms.
- It is not uncommon to get anaemia when you have WM, it is important to make sure you have enough iron in your diet, and get your iron levels checked regularly.
- You may not treatment right away, and may go onto Watch & Wait, or you may have treatment with the aim of going into remission or managing your symptoms and decreasing your IgM levels – rather than being cured from WM.
- Although you will have WM for the rest of your life, you can live well with WM, making healthy life choices can help, and talking to your doctor for advice can be useful.
- If you are interested in joining a clinical trial, talk to your doctor.

