Diagnostic tests are done in the pathology laboratory by specialist doctors and scientists. Tissue samples can include blood tests and tissue biopsies. Sometimes tissue samples may need to be sent to a specialist laboratory at a larger hospital for these tests to be done.
Waiting for the results of some of these tests may sometimes be the reason for the start of the treatment being delayed. It is very important that doctors have all of the information they need to make the best treatment decisions for the patient.
Why are diagnostic tests done?
There are a number of tests that are done to confirm the diagnosis of lymphoma. There are specialist doctors that have undergone special training in this area to interpret these tests from blood, lymph nodes and bone marrow samples to identify disease.
As scientists understand more about lymphoma, new and more sensitive tests are being created to inform doctors about the diagnosis. It is becoming more important for these tests to be performed so they understand the type and behaviour of the lymphoma before deciding on the right treatment for the patient.
In the pathology lab the tissue samples will undergo a number of tests to classify the cancer cells. They also look at their shape, their size and how they are grouped in samples from lymph nodes and bone marrow, by looking under the microscope. They will do additional tests such as immunophenotyping, cytogenetic analysis and/or molecular studies to find out more information to indicate how the lymphoma may behave.
What is Immunophenotyping?
Immunophenotyping is a process used to distinguish between different types of cells. For example, the difference between normal lymphocytes and lymphoma cells. It does this by detecting small identifying substances, called ‘markers’ or ‘antigens’ that are expressed on the cells.
Immunophenotyping gives information on the types of antigens found on or within white blood cells (WBCs). This test can help to diagnose and identify specific types of lymphoma. In some cases, the information can predict how aggressive a lymphoma is or how responsive it will be to treatment. Testing may be done to see how effective treatment has been and to look for any residual or recurrent disease.
Immunophenotyping can be done through two methods. These include a test called immunohistochemistry (IHC) or flow cytometry.
Immunohistochemistry (IHC)
Immunophenotyping can be done through two methods. Immunohistochemistry (IHC), this is where stains are applied to cells that are on a slide. They are then looked at under the microscope. The stains will identify the antigens or markers present on the cells.
Flow cytometry
The other method is flow cytometry. In this test the sample is processed and antibodies that are tagged with fluorescent markers are added. These antibodies attach to specific antigens when they are present. The sample flows through an instrument called a flow cytometry where individual cells are analysed.
Flow cytometry measures the number and percentage of cells in a blood sample and cell characteristics such as size, shape and the presence of biomarkers on the cell surface. Flow cytometry can also detect residual levels of disease after treatment. This helps the doctor identify disease relapse and restart treatment as needed.
Immunohistochemistry (IHC)
- Thin slices of the biopsy sample (or thin layers of fluid) are treated with sets of antibodies that recognise different markers found in different types of lymphoma or leukemic cells and normal lymphocytes.
- The pathologist examines the slides under a microscope to look for the visible colour change that happens when the antibody sticks to the marker
- The pathologist identifies and counts the number of cells that are highlighted by colour (meaning that they are positive for the marker) with each of the different antibodies.
Flow cytometry
- Cells from the biopsy sample are placed in a liquid solution and treated with sets of antibodies that recognise different antigens found in different types of lymphoma cells.
- The cell-antibody mixture is injected into an instrument called a flow cytometer. This machine uses laser beams to sense the different colours the cells emit from the different antibodies attached to them. This information is measured and analysed by a computer and interpreted by a pathologist.
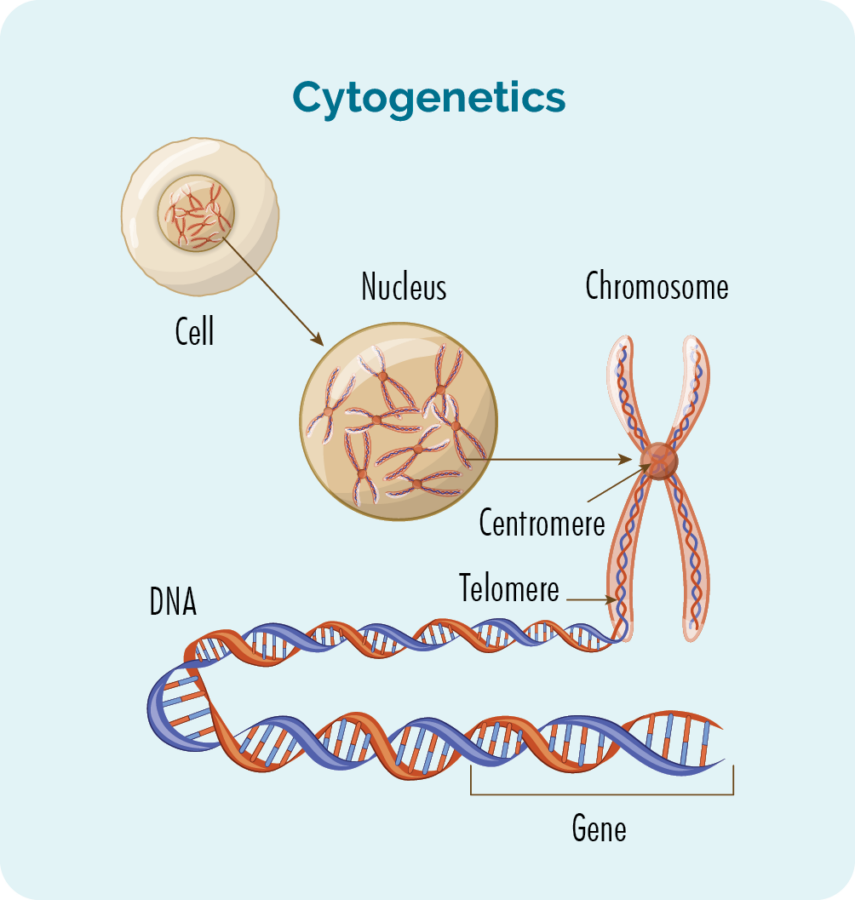
What is cytogenetic analysis?
Chromosomes contain genes that comprise long strands of DNA. Healthy human cells have 23 pairs of chromosomes. Chromosomes are divided into two regions called ‘arms’, which are called p (the short arm) and q (the long arm). Some lymphomas and other types of cancer have too many or too few chromosomes or have chromosomes with an abnormal structure. Most commonly chromosomes are broken and reattached (translocations), so that chromosome pieces are misconnected leading to activation of tumour growth signals.
In cytogenetic analysis, chromosomes from cancer cells are examined under a microscope to check that there are not too few or too many chromosomes. It usually takes two to three weeks to obtain results from cytogenetic testing because a sufficient number of cancer cells must be grown in the laboratory to get enough genetic material for the analysis.
The results of the cytogenetic analysis can also help distinguish between different types of non-Hodgkin lymphoma or help in making treatment decisions.
What are the types of chromosomal abnormalities?
One type of chromosomal abnormality found in some lymphoma types is called translocation, which occurs when part of a chromosome breaks off from its normal location and becomes attached to another chromosome.
Another type of chromosomal abnormality is called a deletion, which happens when part of a chromosome is missing. This is written, for example as del(17p), noting there was a deletion in the short arm of chromosome 17.
Why might a patient need additional genetic tests?
Doctors may order additional genetic tests to confirm the results of cytogenetic tests or to find our more detailed information about the types of damage to the genetic information of the lymphoma cells.
Types of additional genetic tests
Fluorescence in situ hybridization (FISH)
- FISH uses fluorescent chemicals to specifically attach to certain parts of chromosomes to show the presence of translocations and other large abnormalities.
- FISH provides researchers with a way to visualise and map genetic material in an individual’s cells, including specific genes or portions of genes. This may be used for understanding a variety of chromosomal abnormalities and other genetic mutations.
- FISH can be performed on blood, lymph nodes, or bone marrow samples, and test results are usually available within a few days (quicker than cytogenetic testing).
Polymerase chain reaction (PCR)
- PCR is a test that is used to measure specific genes (ie, DNA) that cannot be seen under a microscope.
- PCR tests can be done on a very small quantity of cells, and it usually takes about one week to get these results.
DNA sequencing
- Some abnormalities in tumour growth occur because of changes in the sequence of a specific gene or set of genes
- These findings can help define the type of tumour, determine prognosis, or influence treatment choice.
- An individual gene may be sequenced or a panel of known critical genes can be sequenced at one time.
How will a patient get their results?
These are highly specialised tests done only at certain laboratories. The haematologist will get the results and interpret these with all of the other test results. These tests may take a little while to come back and some tests can take a few days and others can take weeks.
It is important to get some of this information before treatment can start to ensure the right treatment is being given for the individual patient. It is important for patients to know that interpreting diagnostic tests should be done between the doctor and the patient.
What does the report mean?
Some patients like to review their written reports; when doing so, it is important for the patient to carefully review the findings with their doctor. This is because often the doctor interprets many results from different tests to make an informed diagnosis.
This is an example of some of the CD markers for different types of non-Hodgkin lymphomas that the doctors look at to see what the diagnosis of lymphoma, see the table below:
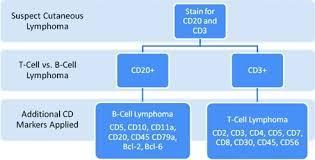
Note: One of the useful markers for the diagnosis Hodgkin lymphoma is CD30

