Aches and pains are a common problem for people with lymphoma and can range from mild to severe. There are several reasons you may get aches and pains, and this page will provide information on why, what you can do to manage it, and when to see your doctor.
What causes aches & pains during lymphoma treatment
Aches and pains may be caused by your lymphoma, procedures you have such as biopsies or insertion of central venous access devices or cannulas, or from the treatment you have. Click on the headings below to learn more.
Lymphoma may not cause any pain at all. Often swollen lymph nodes due to lymphoma are painless. However, you may get pain if your lymph nodes are large, or the lymphoma is putting pressure on other structures in your body such as your bones, organs or nerves.
Inflammation can also happen around the areas of the lymphoma, and this can cause pain too.
There are several procedures you may need during your diagnosis, staging and treatment that can cause some aches and pains. These can include:
- Lymph node biopsy
- Bone marrow biopsy
- Lumbar puncture
- Surgery
- Central venous access device (CVAD) insertion
- Cannulation.
This type of pain should be short-lived, and in most cases won’t need any medical intervention. Cold packs can help reduce inflammation around the surgery or biopsy sites and in doing so, can provide some pain relief.
If cold packs are not enough, paracetamol taken as directed may help.
Avoid anti-inflammatory medicine such as ibuprofen (Nurofen) or aspirin within the first few days of the procedure. These medications can increase bleeding and bruising, and result in more pain.
Let your doctor or nurse know if the above tips don’t work for you. Pain can sometimes be caused by infection, so they will need to assess your wound site. They will also be able to advise whether you need stronger medicine or other treatments to control the pain.
Infection
Always let you nurse or doctor know if you have signs of infection. These can include:
- Pain
- Redness or swelling around a wound or needle site
- Pus or other smelly discharge
- Having a temperature of 38° degrees or more
- Chills or rigors (uncontrollable shaking).
Most treatments for lymphoma can cause some degree of aches and pain because in order for the treatments to work, they need to destroy the lymphoma cells.
The lymphoma cells may be directly destroyed by treatments such as chemotherapy or radiotherapy. Other treatments, such as monoclonal antibodies and immunotherapies engage or target your immune system to help it fight the lymphoma more effectively.
Cell destruction
Side-effects of treatment
Some treatments can cause unwanted side-effects that result in pain. Click on the links below to learn more about how side-effects can cause pain, and how to manage them.
Growth factors are a type of supportive treatment that helps stimulates your bone marrow to make new blood cells.
The extra activity and increased number of cells your bone marrow makes due to these treatments can cause bone pain. As the cells are made your bone marrow expands putting pressure on your bones, before releasing the cells into your blood stream. It usually only lasts a few days, but for some people it can be extreme.
Bone pain can range from mild to severe. Some things you can try to improve this pain include:
- Warm or cold packs
- Gentle exercise and walking
- Paracetamol (also called panadol or panamax)
- Over the counter antihistamine such as loratidine.
Fatigue, time in hospital or feeling unwell can result in you being less physically active. This can cause your muscles to start breaking down or become stiff resulting in pain and aches in your muscles, and the joints supported by your muscles.
Eating a well-balanced diet with protein can help your body recover. Other ways to prevent, or improve this type of aches and pains include gentle exercises and stretches or warm or cool packs.
If exercise is difficult for you, ask your doctor to refer you to an occupational therapist, physiotherapist or exercise physiologist. They will be able to assess your needs and ability, and help you come up with a plan to increase your activity within your limits in a safe way.
Sometimes during or after treatment for lymphoma you may experience pain during sex. This if often caused by vaginal dryness or a lack of lubrication. Try using a lubricant to resolve the pain. If the pain continues, a referral to a Women’s physiotherapist can develop a plan to address the pain.
It is important to be aware that ongoing pain during sex needs to be investigated by a doctor.
Discuss a GP management plan with your doctor as you may be able to access specialist referrals with an occupational therapist, physiotherapist or exercise physiologist with little or no out of pocket cost. These services are then funded by Medicare.
How to manage aches & pains
Exercise & stretches
Research has shown that gentle exercise and stretches can help to improve aches and pains. However, depending on your individual circumstances, you may not be able to keep up with your usual activity levels.
Working out what your new limits are, can take time and you may need advice from a physiotherapist or exercise physiologist. They can help you work out what you can do, and how to do it safely while having treatment for lymphoma.
Sleep
Pain is always harder to cope with when you are tired. Fatigue and lack of sleep may make your aches and pain feel worse or harder to manage. It’s important to manage any fatigue or sleep issues early to avoid developing poor sleep routines. For more information on managing fatigue and sleep issues, click the links below.
- Fatigue (extreme tiredness)
- Sleep issues.
Heat or cold packs
Try experimenting with both heat and cold packs to find what works best for you. You may even find switching between heat and cold works best.
Caution
Some treatments for lymphoma can affect your ability to feel hot and cold properly. This puts you at increased risk of burns. When using heat or cold packs, only heat or freeze as instructed, and always have a towel or clothing between your skin and the heat/cold pack. For more information on this please see our webpage on peripheral neuropathy.
Medicines

Paracetamol
Paracetamol – also known as Panadol or Panamax is usually safe when you have lymphoma however, it can mask a temperature. Always take your temperature before you have paracetamol if you are having treatment for lymphoma.
Paracetamol may not be safe for you if you have problems with your liver. If you’ve been told you have problems with your liver, ask your doctor or nurse if it is safe to take paracetamol.
Anti-inflammatories
Anti-histamines
Histamine is a chemical released by immune cells called basophils and mast cells. These are different types of white blood cells, and the histamine they release triggers inflammation. This is helpful to fight infection, but too much histamine, or in the absence of infection can cause pain. By reducing histamine, you can reduce inflammation and decrease pain levels.
Before taking any over the counter medicine, check with your pharmacist or doctor if it is safe to take in your individual circumstances. Some medicines can interact with cancer treatments, making them less effective, or more likely to cause severe unwanted side-effects. Paracetamol can also be dangerous if your liver is not working properly.
Get the right health professionals involved
There are different health professionals outside of your haemotology on oncology team that can help you manage your pain. Each has different expertise and which ones will be best for you will depend on your individual circumstances.
Click on the headings below to see how the different health professionals or services may be able to help. Talk to your nurse or doctor about getting a referral to any services you think may be of use to you.
***The below information is for people who have a Medicare card. If you do not have a Medicare card, you may have extra costs to pay.
If you haven’t already found a regular local doctor (GP), now is the time to do it. You will need a regular and trusted GP to support you through your treatment, co-ordinate your care and provide important follow-up care after you finish treatment.
GPs can help by prescribing some medicines and referring you to different specialists and health professionals. They can also put together a chronic disease management plan, mental health care plan and survivorship care plan with you.
Talk to your doctor about these plans and how they can help in your individual circumstances.
GP management plan
Cancer is considered a chronic illness because it lasts longer than 3 months. A GP management plan allows you to access up to 5 allied health consults per year with no, or very little out of pocket cost to you. These can include physiotherapists, exercise physiologists and occupational therapists.
To learn more about what is covered by allied health, please see the below link.
Allied health professions – Allied Health Professions Australia (ahpa.com.au)
Mental health management plan
Everyone with cancer should have a mental health plan. They are also available to your family members and provide you with 10 visits or telehealth appointments with a psychologist. The plan also helps you and your GP discuss what your needs will be over the year, and come up with a plan to help you cope with the extra stressors, including pain you are dealing with.
Find more information on what mental health care is available here Mental health care and Medicare – Medicare – Services Australia.
Survivorship care plan
A survivorship care plan helps to coordinate the care you need after a cancer diagnosis. You may have one of these done before you finish treatment, but not always.
A survivorship plan is a great way to look at how you will manage after treatment ends, including managing side-effects such as pain and follow up tests.
A physiotherapist can help in several ways. They can assess your movement and breathing ability and help you come up with a plan to maintain or improve your muscles and flexibility during treatment.
They can also help improve pain with different types of treatment including:
- massage
- safe exercise and stretching
- heat or cold therapies
- acupuncture
- cupping
- hydrotherapy
- ultrasound therapy
- infrared or cold laser therapy
- more.
Exercise physiologists are university trained health professionals that have expertise in the way your body responds to exercise.
They are able to assess how the lymphoma and pain impacts your body and your ability to exercise and find the best exercises to work with you.
Exercise physiologists often work in partnership with physiotherapists. To find an
An occupational therapist can help by assessing how your pain or illness affects your ability to perform activities of daily living (ADLs), such as getting dressed, showering and completing housework.
They can organise special equipment or minor changes to your home to help you perform ADLs more easily.
Many hospitals have an acute pain service that can help if you have complex pain that is not expected to last more than 3 months. Complex pain is pain that persists, even after treatments given by your usual doctor or surgeon.
The Acute Pain Service can organise special pumps with medicine that you can control and take as needed. This is called Patient Controlled Anaesthesia (PCA), or other types of medicine.
Chronic pain service can help with pain that lasts more than 3 months. They may be able to prescribe different types of pain relief in the way of medicine or surgical procedures.
Palliative care teams can help when you’re in hospital or at home. They are experts at managing difficult to treat symptoms and side-effects that do not respond to standard treatments such as pain, anxiety and nausea. Palliative care doctors have the authority to prescribe some medicines or doses that other doctors including haematologists and oncologists may not be authorised to prescribe.
When to see your doctor
Pain is a natural response to injury and can often be managed at home with the above tips. However, there are times when pain should net be ignored or managed at home. Make an appointment to see a doctor if your pain:
- lasts longer than expected
- has affected your sleep for more than 3 nights in a row
- prevents you from completing your activities of daily living
- is concerning you.
Get immediate medical help, or call an ambulance on 000 if your pain:
- is in your chest or radiates to your shoulders, arms or around your back,
- is near a wound or rash that looks infected,
- is extreme and more than you can handle,
- causes weakness in your arms or legs
- makes it difficult to go the toilet, or you become incontinent (not making it to the toilet in time)
- makes you want to hurt yourself,
- or if you also have a temperature of 38° degrees or more.
Summary
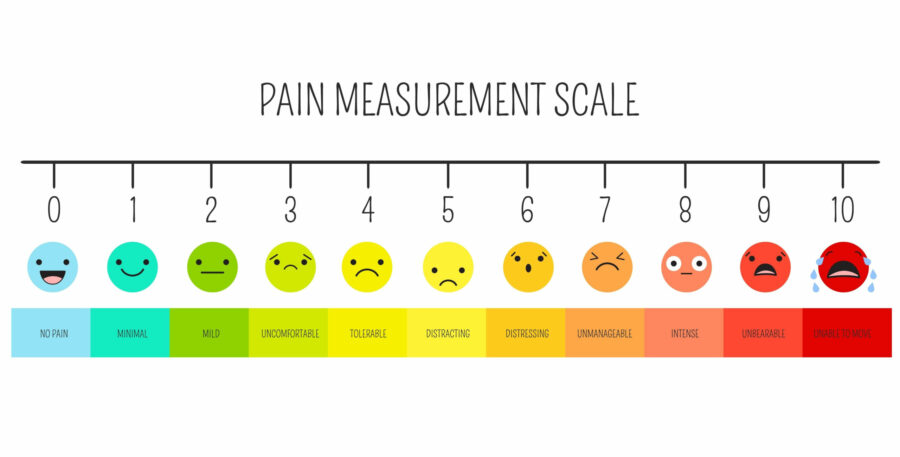
- Pain is common among people with lymphoma, and can range from mild to extreme.
- There are many different reasons you might get aches and pains, most should not last more than a few days, but some can become chronic – lasting more than 3 months.
- Exercise and stretching in a safe way is important when you have lymphoma.
- There are many different health professionals that can help you manage your aches and pains – talk to your doctor about your needs.
- Some over the counter medicine can help improve pain, but talk to your pharmacist first to make sure it is safe to take – some medicine can interact with anti-cancer medicines or cause damage to your liver.
- If natural methods mentioned above, and over the counter medicines are not enough, talk to your doctor about the help available to you to manage the pain.
- Ask your doctor to do a GP management plan with you.
- Seek extra help when needed as listed above.
- Call our Lymphoma Care Nurses if you would like more information – click the Contact us button on the bottom of the screen for details