Changes to your lungs, can happen during or after treatment for lymphoma. Changes to your lungs resulting as a side-effect of treatment are called pulmonary toxicities. These changes can affect your fitness and breathing capacity. You may find you get breathless easier than you did before treatment, or that your fitness isn’t what it used to be.
This webpage will provide information on what changes can happen, why they happen and how they can be managed.
What do our lungs do?
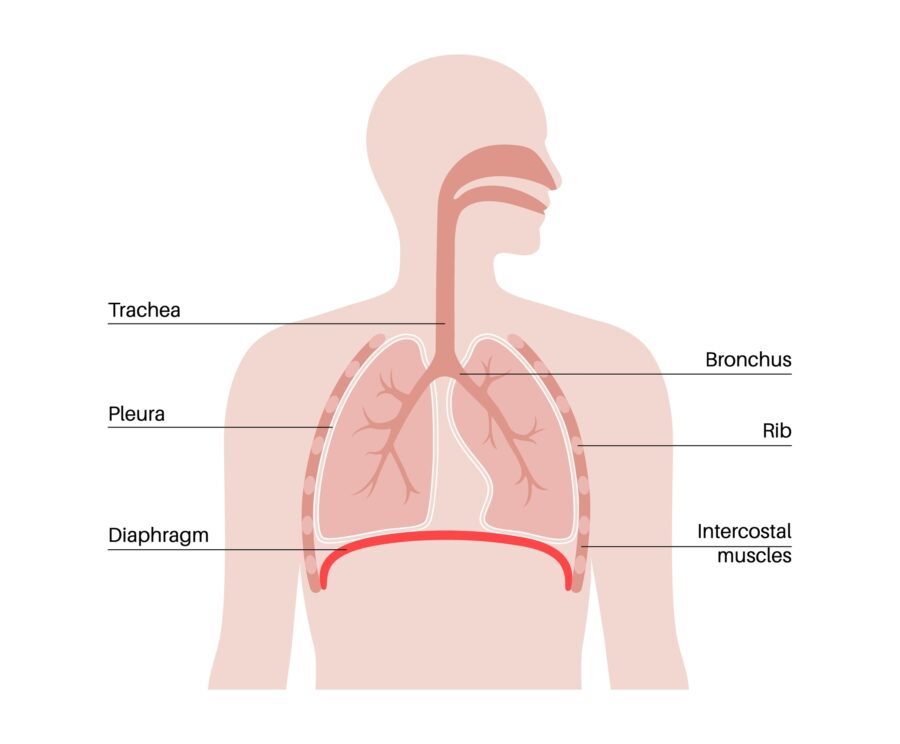
Our lungs are organs that help us breathe. They expand as we breathe in, and contract as we breath out. It is in our lungs that the heamoglobin on our red blood cells pick up oxygen to deliver to the rest of our body, and where the red cells drop off waste products like carbon dioxide for us to breathe out.
We have two lungs, one on the right side and one on the left side of our chest. Because our heart is also on the left side of our chest, the left lung is a bit smaller than the one on the right. Our right lung has 3 segments (called lobes) and the left lung has only 2 lobes.
Other functions of our lungs
The airflow from our lungs is needed for us to speak and regulate our voice.
Our lungs play an important role in protecting us from germs that create infection and disease. B-cell lymphocytes in our lungs produce an antibody called Immunoglobulin A, which helps to fight respiratory infections.
Our lungs also produce a type of mucous that traps and kills germs to prevent them causing infection.
By removing carbon dioxide when we breathe out, our lungs help to stop our body from becoming too acidic. In the short term, if our bodies become too acidic we can have:
- fast heart beat
- fatigue and weakness
- dizziness
- confusion
- nausea and vomiting or loss of appetite.
However, if our bodies remain too acidic long term we can be at more risk of certain conditions and diseases including:
- tooth decay
- cancer
- heart disease
- allergies
- damage to our throat or stomach
- obesity
- problems with our nervous system, heart or muscles.
What causes lung changes?
Some lymphomas and treatments for lymphoma can cause changes to your lungs.
Lymphoma
Primary mediastinal lymphoma starts in the middle of your chest (mediastinum) and can affect your lungs. Many people with Hodgkin Lymphoma may also have it start in their mediastinum. And others may have lymphoma that spreads to the chest or puts pressure on your lungs. Some lymphomas may even start in your lungs.
These lymphomas may all affect your lungs if they are large enough to put pressure on them, and stop them from expanding fully when you breathe in, or contracting when you breathe out. If your lymphoma is in your lungs, it may affect the way they work.
Treatments that may cause pulmonary toxicity
Although chemotherapy is very effective at fighting many lymphomas, some chemotherapy medicines can case pulmonary toxicities.
Bleomycin
Bleomycin is a chemotherapy commonly used to treat Hodgkin Lymphoma and can rarely cause lung changes. However, the risk of pulmonary toxicity related to bleomycin is increased if you:
- over 40 years old
- smoke
- have other lung conditions
- have problems with your kidneys.
High dose oxygen is often used in hospitals or during scuba diving. If oxygen is needed in hospital you may be offered medical air rather than high dose oxygen. Make sure you always let your doctors and nurses know that you have had bleomycin, even if you had it years ago. They will likely list oxygen as an allergy to make sure you are not given high-dose oxygen.
It is a good idea to carry a card or have a wrist band or bracelet to let people know you cannot have high-dose oxygen in case you are ever in a situation that you cannot communicate it yourself.
Bleomycin is commonly used in the chemotherapy protocols ABVD and eBEACOPP.
Other chemotherapies
Other chemotherapies that may cause pulmonary toxicities are listed below. However, it is important to remember that these side effects are rare, and most people receiving treatments will not develop pulmonary toxicity.
- methotrexate
- gemcitabine
- busulfan
- carmustine
- melphalan
- cyclophosphamide
- chlorambucil
- cytarabine
- platinum based chemo’s such as cisplatin or carboplatin.
Unlike with bleomycin, if your pulmonary toxicity is caused by a different type of chemotherapy you will still be able to use high-dose oxygen if needed without added risk.
Radiotherapy can increase your risk of pulmonary toxicities if the radiation is to your chest, mediastinum or lungs. The risk is higher if you have also had or, are having chemotherapy as well.
Some immunotherapies can also cause pulmonary toxicities. These include monoclonal antibodies commonly used in treatment for lymphoma such as rituximab, obinutuzumab and brentuximab vedotin.
Immune checkpoint inhibitors such as pembrolizumab and nivolumab can cause an immune reaction within your lungs that results in your immune system not recognising the cells in your lungs as being art of you. So instead, your immune system can view these cells as a germ and may attack them. These sorts of reactions need to be treated differently from pulmonary toxicities caused by other treatments and usually includes steroids to stop the immune reaction.
Symptoms of lung changes
You need to report all new, or worsening symptoms to your doctor or nurse so they can assess you. In many cases, you may not need any treatment but if you do, delaying treatment can become very serious quickly. Many lung toxicities may be temporary and need no, or only short-term treatment. Rarely, pulmonary toxicities have lasting effects that will become a permanent health condition.
Symptoms you may experience with pulmonary toxicities include:
- difficulty breathing
- shortness of breath for no reason
- wheezing or noisy breathing
- changes to your voice or difficulty speaking
- dizziness or confusion
- tingling under your skin
- coughing
- chest pain
- a bluish colour around your lips, fingers or toes
- worsening of any existing lung conditions such as asthma or chronic obstructive pulmonary disease (COPD).
When to see your doctor
Contact your doctor for a review if you get any of the above symptoms. If you are seeing your GP (local doctor) or doctor other than your haematologist of oncologist let them know what:
- symptoms you’re getting, when they started and if they have gotten worse,
- what treatment you are having and when you last had it.
Call an ambulance or get to your nearest emergency department if you have a temperature of 38 degrees or more, if you have chest pain, if you become very short of breath, or if you become very unwell.
How are lung changes diagnosed?
Your doctor will do a physical examination and listen to your lungs. They will then look other things like when you last had treatment and what treatment you had, recent blood tests and other medicines you might be taking. Once they have the full picture, they wll determine what extra tests you may need. These may include:
- chest X-ray
- CT or MRI of your chest
- sputum test
- pulmonary function test
- bronchoscopy
- blood tests.
Treatment for lung changes
Treatment for pulmonary toxicity and other lung changes will depend on the type of treatment you’ve had, the severity of your symptoms and the type of lung changes that have happened.
Pulmonary toxicity from treatments
When lung changes occur as a result of pulmonary toxicity caused by your treatments, you may be offered:
- Medicine such as steroids, antihistamines, ventolin or sulbutamol. Medicine may be ordered to have as a tablet, intravenously (into your vein), as a puffer or nebuliser (to be breathed in).
- Antibiotics, antifungal or antiviral medicine if you have, or are at risk of getting a lung infection.
- Chest physiotherapy and exercises
- Extra time before next treatments.
Lung changes from lymphoma
Lung changes that happen as a result of lymphoma in your chest or lungs will be managed differently from pulmonary toxicity. When the lymphoma is the cause of your lung changes, the treatment will be to shrink the lymphoma to prevent the pressure on or in your lungs. This means, that you will need treatment such as chemotherapy, radiation or surgery to remove or shrink the lymphoma.
As the lymphoma gets smaller or is removed your lungs should start to function properly again, improving your symptoms.
Living with lung changes
When lung changes become permanent it can affect many areas of your life. It can take some time to recover and learn what your new capacity is, and how to live within your limits. You may have new medicines you need to take, or extra appointments at the hospital.
Things you can do to improve your quality of life with lung changes include:
- Get a mental health plan from your GP to help cope with fear, anxiety or added stress you have because of these changes.
- Get a GP management plan with your local GP. These plans can provide you with 5 allied health appointments at no, or very little cost to you. These can include dietician, exercise physiologist, physiotherapist, occupational therapist and more.
- Maintain a healthy weight for your height. A dietician can help with this if you are under or overweight, or want to learn more about healthy eating.
- Exercise regularly – an exercise physiologist can help you work out an exercise routine that you enjoy and can manage.
- See a physiotherapist for lung strengthening exercises.
- Have an occupational therapist review your home and activities to see how they can help you manage your activities of daily living with less stress on your lungs.
Summary
- Lung changes can happen as a symptom of your lymphoma or as a side-effect of treatment.
- Lung changes caused by your treatments are called pulmonary toxicity.
- Pulmonary toxicities are rare and can be temporary or permanent.
- Report all new or worsening symptoms to your doctor. Let them know what treatment you had, when you last had it, and ALWAYS tell your doctors and nurses if you have EVER had bleomycin or an immune checkpoint inhibitor such as pembrolizumab or nivolumab.
- Call an ambulance if you have a temperature of 38° degrees or more, have chest pain, become very short of breath or are very unwell.
- You may need to see another doctor called a respiratory physician to manage your lung changes.
- Treatment will depend on the type of changes you have, your symptoms and the treatment you have had.
- Get your GP to do a mental health plan and a GP management plan if you have long term changes to lungs or would like extra help even if your lung changes are temporary.
- Call our Lymphoma Care Nurses if you would like to talk through your symptoms or would like more information. Click on the contact us button at the bottom of the screen for contact details.

